Developing New Techniques: Ultrasound-Guided Penile Nerve Block for Circumcision: A Modified in-Plane Technique
By M-Irfan Suleman, MD
This technique was undertaken while the author was faculty at:
Assistant Professor of Anesthesiology
Director of Pediatric Regional Anesthesia
Department of Anesthesiology
Arkansas Children’s Hospital and University of Arkansas for Medical Sciences
Little Rock, Arkansas
No relevant financial disclosures.
Dr. Suleman describes a modified, ultrasound-guided penile block for male pediatric patients undergoing circumcision. The technique uses portable ultrasound with a linear probe and real-time scan at the base of the penis to identify vessels and fascia layers, which allows safe advancement of the needle and injection of local anesthesia bilaterally. The technique allows the practitioner to see local anesthetic distribution under the deep fascia of the penis. This procedure produces a subcutaneous wheal along the anterior side of the base of the penis at the penoscrotal junction and seems to improve the success rate of achieving a complete penile block (Figure 1).
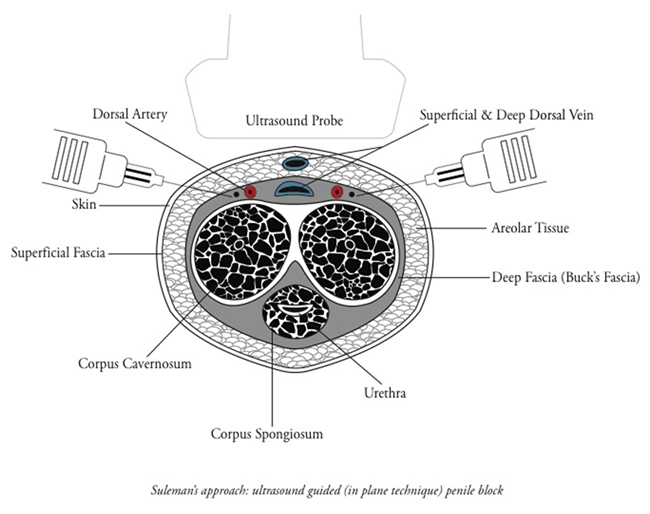
Figure 1: Suleman approach schematic
Introduction
Circumcision is one of the most frequent surgical procedures for pediatric males.1,2 In an effort to relieve postoperative pain, several analgesic approaches, all with varying efficacies, have been used, including topical analgesics such as lidocaine and lidocaine-prilocaine,3-6 ring block,7-9 and caudal block.5,8,10 A study by Weksler et. al found that children treated with caudal block had an increased incidence of tachycardia, motor block, and vomiting compared with those treated with penile block, without a significant difference in pain severity between the groups.11 The ring block procedure includes an 8% failure rate,8 bleeding,12 and edema,13 although complications have not been reported with this technique.2
Landmark-based needle placement, described by Maxwell et al,17 has been a standard method to block the dorsal penile nerve. However recently, interest has focused on using ultrasound to direct bilateral injections into the subpubic space,14 thus allowing clearer identification of both the subpubic space and penile structures,15 although some researchers remain unconvinced of this procedure’s benefits.16
Ultrasound guidance verifies the distribution of the anesthetic in real time.15 In addition, ultrasound guided technique has lowered postoperative pain scores14,18 and shortened recovery time.18 Identification of better techniques could make ultrasound-guided regional anesthesia a standard of care for this application. With this technology relief of patient’s discomfort and better pain control is achieved as a part of perioperative care for circumcision.
Methods
I describe a modified, ultrasound-guided penile block for male children undergoing circumcision. After administering general anesthesia to the patient, the penis and surrounding area, including the scrotum, was prepped with 0.5% chlorhexidine in 70% alcohol. Sterilized gel was used at the site and the ultrasound probe was covered to ensure sterility, 4-inch sterile occlusive dressing was used, which is easier to apply and less costly than commercial probe covers (Figure 2).

Figure 2: Suleman approach: ultrasound-guided (in-plane technique) penile block
Holding the ultrasound probe while positioning the needle against the probe can be problematic, but I found that the 27-gauge, 1.5-inch regular hypodermic needle is comfortable to use and easily visible on the ultrasound monitor because the nerve is close to the skin. Sandeman and Dilley15 recognized that observing the tissue movement as the needle advances and checking for the dark, hypoechoic region on the ultrasound monitor indicate both the needle tip position and placement of the anesthetic; I found this to be accurate as well, but prefer an in-plane technique to see needle advancement to avoid any surrounding structures.
A linear ultrasound probe with a frequency range of 5 to 10 MHz with musculoskeletal setting was used for optimal viewing on the monitor. The probe was placed transversely along the base of the penis using gentle traction. The corpora cavernosa, dorsal arteries, dorsal veins, and superficial and deep penile Buck’s fascia were identified. The needle was moved forward using the in-plane technique under real-time ultrasound guidance and continued to advance until the practitioner felt a loss of resistance as the needle passed through the hyperechoic superficial lining of Buck’s fascia. Immediately after passing through this superficial layer, the needle tip, located lateral to the dorsal artery, was advanced deep into Buck’s fascia. After negative aspiration, I injected 1 to 2 mL of local anesthetic under direct vision,19 while monitoring to avoid neurovascular injury or intravascular injection20 .
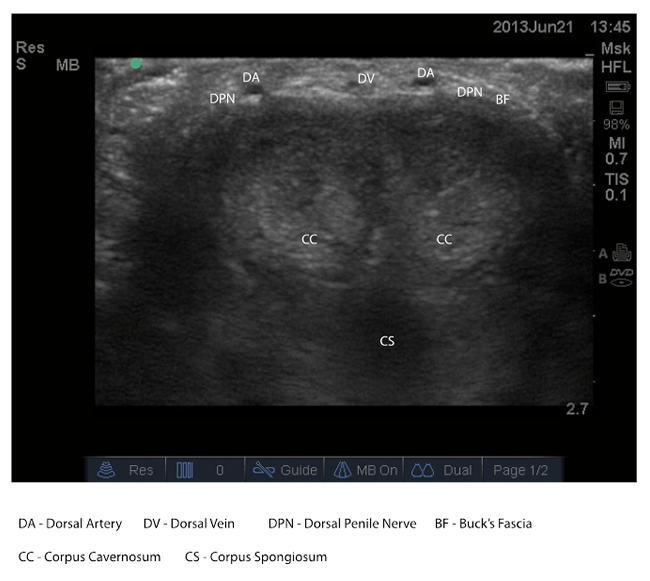
Figure 3: Suleman approach showing ultrasound-guided landmarks for dorsal penile nerve block
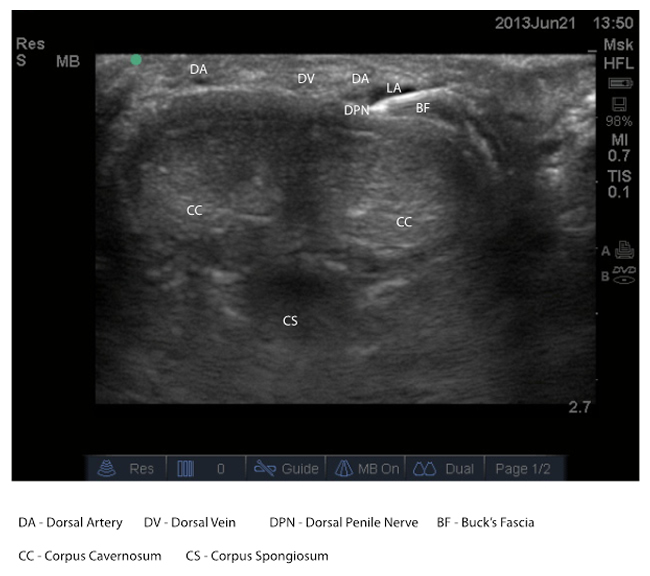
Figure 4: Suleman approach showing ultrasound-guided in-plane needle placement for dorsal penile nerve block
Plain 0.25% bupivacaine, 3 ml was injected. The local anesthetic spread was evident on ultrasound as a hypoechoic area, and the same procedure was repeated on the other side. Finally, I placed a small ventral bleb with local anesthetic at the penoscrotal junction to block the scrotal branches of the pudendal nerve, as recommended by Sandeman and Dilley.15
Discussion
Dorsal penile nerve block (DPNB), a procedure first described in the mid-1970s,21 requires a local anesthetic injection close to the dorsal nerve of the penis. The American Academy of Pediatrics approves the use of DPNB.2 Reports of minor complications include swelling,22 hematoma or edema,23 and bruising at the injection site.24 Other safe approaches using DPNB in infants and children have been described.13,25
Ultrasound imaging in regional anesthesia is a leading advancement in improving safety of pediatric regional anesthesia.26 The technology allows the practitioner to visualize the target nerve directly, maneuver the needle under real-time observation, precisely navigate away from complex or sensitive anatomy, and manage and administer the distribution of local anesthetics.
For those who believe that DPNB is an uncomplicated procedure that does not require routine ultrasound,16 I argue that ultrasound allows the two-dimensional anatomy of the subpubic space and penile structures to be clearly recognized, allowing needle placement directly into the subpubic space, thus avoiding the penile structures and problems that could occur.
Several studies have concluded that when needles are placed close to the nerves, the frequency of adverse events declines.15,18,27 In-plane needle placement technique seems to be reliable and minimizes adverse events and is simple to learn. I recommend this ultrasound technique to improve clinical care for patients undergoing circumcision.
References
- Al-Ghazo MA, Banihani KE. Circumcision revision in male children. Int Braz J Urol. 2006;32:454-458.
- American Academy of Pediatrics, Technical report: Male circumcision. Pediatrics. 2012;130:e756-e785.
- Benini F, Johnston CC, Faucher D, et al. Topical anesthesia during circumcision in newborn infants. JAMA. 1993;270:850-853.
- Choi WY, Irwin MG, Hui TW, et al. EMLA cream versus dorsal penile nerve block for postcircumcision analgesia in children. Anesth Analg. 2003;96:396-399.
- Tree-Trakarn T, Pirayavaraporn S. Postoperative pain relief for circumcision in children: comparison among morphine, nerve block, and topical analgesia. Anesthesiology. 1985;62:519-522.
- Woodman PJ. Topical lidocaine-prilocaine versus lidocaine for neonatal circumcision: a randomized controlled trial. Obstet Gynecol. 1999;93:775-779.
- Broadman LM, Hannallah RS, Belman AB, et al. Post-circumcision analgesia--a prospective evaluation of subcutaneous ring block of the penis. Anesthesiology. 1987;67:399-402.
- Irwin MG, Cheng W. Comparison of subcutaneous ring block of the penis with caudal epidural block for post-circumcision analgesia in children. Anaesth Intensive Care. 1996;24:365-367.
- Lander J, Brady-Fryer B, Metcalfe JB, et al. Comparison of ring block, dorsal penile nerve block, and topical anesthesia for neonatal circumcision: a randomized controlled trial. JAMA. 1997;278:2157-2162.
- Bengisun AK, Ekmekci P, Haliloğlu AH. Levobupivacaine for postoperative pain management in circumcision: caudal blocks or dorsal penile nerve block. Ağri. 2012;24:180-186.
- Weksler N, Atias I, Klein M, et al. Is penile block better than caudal epidural block for postcircumcision analgesia? J Anesth. 2005;19:36-39.
- Kaplan GW. Complications of circumcision. Urol Clin North Am. 1983;10:543-549.
- Holder KJ, Peutrell JM, Weir PM. Regional anaesthesia for circumcision. Subcutaneous ring block of the penis and subpubic penile block compared. Eur J Anaesthesiol. 1997;14:495-498.
- Faraoni D, Gilbeau A, Lingier P, et al. Does ultrasound guidance improve the efficacy of dorsal penile nerve block in children? Paediatr Anaesth. 2010;20:931-936.
- Sandeman DJ, Dilley AV. Ultrasound guided dorsal penile nerve block in children. Anaesth Intensive Care. 2007;35:266-269.
- O’Sullivan MJ, Mislovic B, Alexander E. Dorsal penile nerve block for male pediatric circumcision—randomized comparison of ultrasound-guided vs anatomical landmark technique. Paediatr Anaesth. 2011;21:1214-1218.
- Maxwell LG, Yaster M, Wetzel RC, et al. Penile nerve block for newborn circumcision. Obstet Gynecol. 1987;70:415-419.
- Sandeman DJ, Reiner D, Dilley AV, et al. A retrospective audit of three different regional anaesthetic techniques for circumcision in children. Anaesth Intensive Care. 2010;38:519-524.
- Brown TC, Weidner NJ, Bouwmeester J. Dorsal nerve of penis block—anatomical and radiological studies. Anaesth Intensive Care. 1989;17:34-38.
- Soh CR, Ng SB, Lim SL. Dorsal penile nerve block. Paediatr Anaesth. 2003;13:329-333.
- Bateman DV. An alternative block for the relief of pain of circumcision. Anaesthesia. 1975;30:101-102.
- Kirya C, Werthmann MW Jr. Neonatal circumcision and penile dorsal nerve block—a painless procedure. J Pediatr. 1978;92:998-1000.
- Serour F, Cohen A, Mandelberg A, et al. Dorsal penile nerve block in children undergoing circumcision in a day-care surgery. Can J Anaesth. 1996;43:954-958.
- Snellman LW, Stang HJ. Prospective evaluation of complications of dorsal penile nerve block for neonatal circumcision. Pediatrics. 1995;95:705-708.
- Dalens B, Vanneuville G, Dechelotte P. Penile block via the subpubic space in 100 children. Anesth Analg. 1989;69:41-45.
- Griffin J, Nicholls B. Ultrasound in regional anaesthesia. Anaesthesia. 2010;65 Suppl 1:1-12.
- Rubin K, Sullivan D, Sadhasivam S. Are peripheral and neuraxial blocks with ultrasound guidance more effective and safe in children? Paediatr Anaesth. 2009;19:92-96.