AAP Update
Report from the AAP
 By Rae Brown, MD
By Rae Brown, MD
Chair, Section on Anesthesiology and Pain Medicine the American Academy of Pediatrics
The development of Pediatric Pain Medicine (PPM) as a recognized subspecialty continues apace. Within the last two years the SPPM and the Section on Anesthesiology and Pain Medicine have worked together to advance this unique area of medicine. We are much further along in the process than we were two years ago. In some respects, our progress has been astounding.
We have recognized the multidisciplinary nature of PPM and the clear differences from the treatment of pain in adults. As a professional organization, the SPPM has been involved in discussions with other similar organizations (AAP, APS, IASP) and has begun to integrate all of our colleagues with interests in the care of children with complex pain into a subspecialty that, in ten years, will be a mature organization, likely unrecognizable from the current form. The work that SPPM has done in the last year to offer membership to non-physicians with interest in PPM will be invaluable to the future growth of the specialty.
Extending a hand to other groups, often against a prevailing wind, has not been easy, but it assures ongoing progress. PPM is not a field that will be well served by exclusion. It will require our best efforts to continue the work of inclusion – physicians, nurses, psychologists, physical therapists – into a single dynamic specialty. We must take the unique knowledge, and skill sets from each of these groups and others to produce a sophisticated and efficient workforce recognized for excellence in the care of complex pediatric disease processes. The leadership of the SPPM is to be congratulated for the very positive role that they have played.
In conjunction with the SPPM, the AAP, and under the leadership of Dr. Bill Zempsky from the Connecticut Children's Hospital a group has been formed to explore the future progression of PPM as a specialty. Dr. Zempsky, a pediatric emergency medicine physician, has a long and very successful history in treating pain in children and in investigating unique approaches to pain management. His work has been marked by multidisciplinary approaches to pain management, and this makes him an excellent choice to lead the group. As I have reported in the past, principals of the ABA and the ABP are working with this group. At some point, the work of the group would be expected to consider an approach to ACGME recognition for PPM and perhaps a structure for Board certification – either through the American Board of Anesthesiology, the American Board of Pediatrics or both. The group has obtained funding from the Mayday foundation to offset the initial costs of this work; another singular success. There are other groups within the Pediatric Anesthesia and Pediatric Pain Community that have an interest in the outcome of this work. It should be our goal that no group is excluded, and every voice is heard.
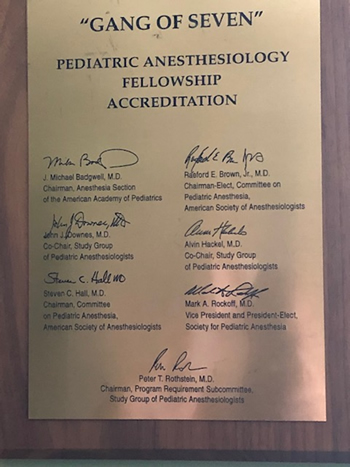 The work of moving a specialty forward is difficult and takes time. I often reflect on my experience with the process of creating the Board-Certified Specialty of Pediatric Anesthesia. A group of seven (Hall, Brown, Rockoff, Downes, Badgwell, Hackel, Rothstein) met in Chicago in 1995 to begin the process of obtaining Fellowship Accreditation for Pediatric Anesthesia programs as a first step to Board Certification.
The work of moving a specialty forward is difficult and takes time. I often reflect on my experience with the process of creating the Board-Certified Specialty of Pediatric Anesthesia. A group of seven (Hall, Brown, Rockoff, Downes, Badgwell, Hackel, Rothstein) met in Chicago in 1995 to begin the process of obtaining Fellowship Accreditation for Pediatric Anesthesia programs as a first step to Board Certification.
This work met resistance from within and outside of the community of Pediatric Anesthesiologists. Despite this, by 2013 the first Certificates of Board Certification in Pediatric Anesthesiology were created by the American Board of Anesthesiology after an approved certification exam of candidates from ACGME approved fellowships. I recount this story because the current process will be just as arduous, and we will question ourselves along the way. That said, for us to provide the best possible care to our patients, this is the road that we must travel.
The work of reducing the risk of harms from opioids in children and adolescents continues. We have worked for the last four years to prevent the further expansion of the number of opioid formulations (currently there are 896 approved formulations listed in the Orange Book of Drug Approval). The industry continues to apply pressure to market increasingly more potent, divertible, and addictive formulations. The FDA has not been supportive of our efforts despite the continued mortality reports and continued prescribing behavior that is more than historical norms. For those of us that advocate for children, the continued presence of opioids in the environment, whether prescribed to adolescents or not has risk harm from diversion. In Kentucky, we continue to bury children because of opioid poisoning. I have worked to understand the particular sensitivity of adolescents to opiate addiction. I will be presenting some of my work in this area at the SPPM meeting in Houston.
We have worked to expand the availability of naloxone, reducing the regulatory oversight and working with the federal government to act as a primary provider of this rescue agent to first responders and to the public. This is our best opportunity, at this time to save lives. Also, we are working with the Agency on the approval of an over the counter formulation.
The creation of a new specialty, the expansion of Pain Medicine to include all interested parties, and the prevention of harm to children are areas where the SPPM and the Section on Anesthesiology and Pain Medicine of the AAP have worked hand in hand in the last year. We should all be proud of this progress, and I would like to thank the President of the SPPM, Anjana Kundu MD, the Vice President, Rita Agarwal, MD and the Executive Committee for their tireless support of this effort.