Non-Opioid Pharmacology in Pediatric Pain Management
Acetaminophen and NSAIDs in Pediatric Pain Management
By Nicholas E. Burjek, MD and Patrick K. Birmingham, MD, FAAP, FASA
Department of Pediatric Anesthesiology
Ann & Robert H. Lurie Children's Hospital of Chicago
Northwestern University Feinberg School of Medicine
Chicago, Illinois
Acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) represent the most used non-opioid pain medications in children. They are well tolerated with limited side effects when used appropriately. Notably, they have less potential for abuse, and represent some of the only analgesics available that do not cause sedation, especially when co-administered with opioids.
Most parents are familiar with these medications and may be less anxious about their use compared to other analgesics that may be perceived as “stronger” or “more dangerous”. Parent and patient familiarity are also beneficial when developing an analgesic plan for use in the outpatient setting. These advantages make acetaminophen and NSAIDs the preferred choice for the management of mild pain in children, and valuable components of a multimodal analgesia plan when treating more severe acute and chronic pain.1,2
Advantages of Acetaminophen/NSAIDs
NON-SEDATING |
LESS ABUSE POTENTIAL |
MEDICATION FAMILIARITY TO FAMILY |
LOW COST |
"OVER THE COUNTER" AVAILABILITY |
Acetaminophen
The mechanism of action for acetaminophen remains an ongoing topic of investigation. Current evidence suggests it inhibits prostaglandin synthesis and activates cannabinoid receptors in the central nervous system, leading to analgesia through activation of descending serotonergic pathways.3 Numerous studies in children have found acetaminophen to be a useful analgesic for a variety of conditions.4 Acetaminophen is safe in appropriate doses, even when used for brief periods in patients with hepatic impairment, but excessive intake may lead to hepatic toxicity and acute liver failure through accumulation of the metabolite N-acetyl-p-benzoquinoneimine. Recommended dosing schedules and maximum daily doses are presented in Table 1.
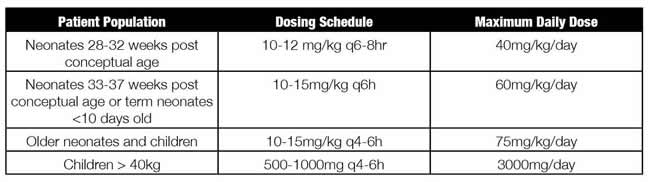
Table 1: Recommended oral acetaminophen dosing and maximum cumulative daily dose in pediatrics.14
Acetaminophen is available as a tablet and oral suspension, which allows easy administration for patients of any size. For patients unable to tolerate oral medications, rectal administration has traditionally been the favored route. However, rectal formulations are available in limited doses, have slower and more variable absorption, and may require a large loading dose followed by higher maintenance doses to achieve adequate analgesia.5 Despite lower expected plasma levels, the maximum daily doses shown in Table 1 should not be surpassed, which complicates the utility of rectal acetaminophen.
Recently available intravenous acetaminophen results in more reliable blood levels than seen with rectal administration and is becoming the preferred route for non-oral administration to hospital inpatients. Optimal dosing of intravenous acetaminophen remains unclear, with some experts recommending a lower maximum daily dose and avoidance in premature infants less than 32 weeks postconception.6 Intravenous acetaminophen remains significantly more expensive than oral formulations, and there is no evidence to suggest improved analgesia via this route. Therefore, for safety and economic reasons, oral administration remains the preferred route for patients able to take medications by mouth.7
Patients may unknowingly take additional sources of acetaminophen in the form of combination drugs, which may lead to inadvertent overdose. Examples include fixed dose combinations with opioids, such as Hycet® (acetaminophen and hydrocodone), and common over-the-counter cold remedies (which often contain decongestants and cough suppressants). All medications being taken by a patient, including those available without a prescription, should be carefully reviewed before recommending acetaminophen. Because fixed dose combinations also limit flexibility in opioid administration, we prefer the use of uncombined opioids when necessary. This allows the patient to take acetaminophen on a scheduled basis, and the opioid or other analgesic only as needed. This also allows patients to take an additional opioid dose without approaching toxic levels of acetaminophen.
NSAIDs
NSAIDs are a varied class of medications that inhibit prostaglandin synthesis through the cyclooxygenase (COX) pathways: COX-1 and COX-2. Prostaglandins cause tissue inflammation and hyperalgesia in the periphery, spinal cord, and brain. Thus, COX inhibition with NSAIDs results in analgesia, decreased inflammation, and fever reduction.
COX enzymes are present in multiple tissue types where they have a variety of roles. As a result, there are several important side effects and contraindications for NSAIDs. Inhibition of COX-1 decreases the protective mucus lining of the stomach, causing a risk of dyspepsia, ulcers, and GI bleeding. NSAIDs also inhibit platelet aggregation through COX-1 inhibition and are therefore often avoided after surgical procedures with a risk of postoperative bleeding. Patients with kidney disease or reduced cardiac output are at risk for worsened renal impairment due to NSAID-induced vasoconstriction of the renal afferent arterioles.
Evidence from animal models has led to a concern that NSAIDs may interfere with osteogenesis. However, studies of children receiving them after spinal fusion or operative fracture repair do not appear to be at increased risk for bone nonunion, and we routinely use NSAIDs following these procedures.8,9 Aspirin, a unique NSAID that irreversibly inhibits COX-1 and COX-2, should not be routinely used as an analgesic in any patients under the age of 18 due to the risk of Reye’s syndrome, a serious acute encephalopathy.10
NSAIDs are effective analgesics for a variety of pain states, and may be more effective than opioids or acetaminophen for mild traumatic musculoskeletal pain.11 When taken for acute postsurgical pain, NSAIDs produce analgesia equivalent to a dose of opioid, and their use with or without additional opioids has been associated with less nausea, vomiting, respiratory depression, and other adverse events.2,12,13 There are a number of NSAIDs available in tablet, suspension, intravenous, and intramuscular formulations, with common doses shown in Table 2. Celecoxib, which is relatively selective in its inhibition of COX-2, has equal analgesic effects compared to other NSAIDs, and may have a lower risk of GI complications.
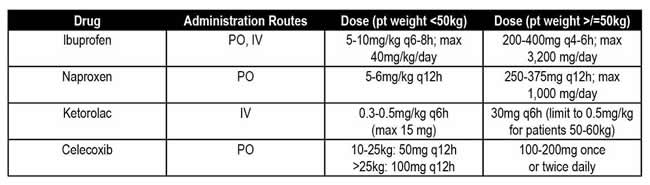
Table 2: Recommended NSAID administration routes and doses in pediatrics
Despite the development of newer analgesics, acetaminophen and NSAIDs remain popular and useful. They provide effective analgesia for a variety of conditions, especially when used together on an alternating schedule.1,4 Certain contraindications exist, but when dosed correctly in appropriate populations they have minimal side effects. Given their availability, effectiveness, variety of administration routes, and lack of interactions with other pain medications, acetaminophen and NSAIDs should be considered when developing any multimodal analgesia strategy.
References
- WHO Guidelines Approved by the Guidelines Review Committee. In: WHO Guidelines on the Pharmacological Treatment of Persisting Pain in Children with Medical Illnesses. Geneva: World Health Organization.; 2012.
- Voepel-Lewis T, Wagner D, Burke C, et al. Early adjuvant use of nonopioids associated with reduced odds of serious postoperative opioid adverse events and need for rescue in children. Paediatr Anaesth. 2013;23(2):162-169.
- Anderson BJ. Paracetamol (Acetaminophen): mechanisms of action. Paediatr Anaesth. 2008;18(10):915-921.
- Zhu A, Benzon HA, Anderson TA. Evidence for the Efficacy of Systemic Opioid-Sparing Analgesics in Pediatric Surgical Populations: A Systematic Review. Anesth Analg. 2017;125(5):1569-1587.
- Birmingham PK, Tobin MJ, Fisher DM, Henthorn TK, Hall SC, Cote CJ. Initial and subsequent dosing of rectal acetaminophen in children: a 24-hour pharmacokinetic study of new dose recommendations. Anesthesiology. 2001;94(3):385-389.
- van den Anker JN, Tibboel D. Pain relief in neonates: when to use intravenous paracetamol. Arch Dis Child. 2011;96(6):573-574.
- Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131-157.
- Munro HM, Walton SR, Malviya S, et al. Low-dose ketorolac improves analgesia and reduces morphine requirements following posterior spinal fusion in adolescents. Can J Anaesth. 2002;49(5):461-466.
- Kay RM, Directo MP, Leathers M, Myung K, Skaggs DL. Complications of ketorolac use in children undergoing operative fracture care. J Pediatr Orthop. 2010;30(7):655-658.
- Glasgow JF. Reye's syndrome: the case for a causal link with aspirin. Drug Saf. 2006;29(12):1111-1121.
- Clark E, Plint AC, Correll R, Gaboury I, Passi B. A randomized, controlled trial of acetaminophen, ibuprofen, and codeine for acute pain relief in children with musculoskeletal trauma. Pediatrics. 2007;119(3):460-467.
- Watcha MF, Jones MB, Lagueruela RG, Schweiger C, White PF. Comparison of ketorolac and morphine as adjuvants during pediatric surgery. Anesthesiology. 1992;76(3):368-372.
- Lewis SR, Nicholson A, Cardwell ME, Siviter G, Smith AF. Nonsteroidal anti-inflammatory drugs and perioperative bleeding in paediatric tonsillectomy. Cochrane Database Syst Rev. 2013(7):Cd003591.
- Lexicomp Online. Acetaminophen. In: Hudson, Ohio: Wolters Kluwer. Accessed January 27, 2020.




