Paravertebral Catheters Underappreciated and Underutilized in Controlling Thoracic and Flank Surgical Pain
 By Mark E. Thompson, MD
By Mark E. Thompson, MD
Covenant Children's Hospital, Lubbock, TX
Assistant Professor Pediatrics and Anesthesiology TTUHSC, Lubbock, TX
Introduction:
Over the last two decades, large registries of pediatric regional experience, such as the French-Language Society of Pediatric anesthesia ADARPEF registries, report a trend away from epidural catheters and toward peripheral nerve blocks for acute pain control. Simultaneously, increasing focus on the potentially neurotoxic effects of inhalational and intravenous anesthetics has increased the role of intraoperative neural blockade as a general anesthetic reduction technique.
The thoracic paravertebral block (TPVB) can be used instead of an epidural in many situations, but is incorrectly considered to be a peripheral nerve block. Epidural spread and even contralateral spread is known to occur with TPVB, although exact incidence depends on needle approach and catheter deployment technique. Contained within the paravertebral space are the spinal nerve roots which are invested by, and continuous with, the dural sleeve of the spinal canal, as well as the sympathetic chain. A variety of synonyms correctly describe this block as extraneuraxial, nerve root level, or paravertebral.
TPVB was described in the early 1900's and variably used for post-thoracotomy pain. Catheters were typically placed by the surgeon under direct visualization prior to wound closure. TPVB was not widely used by anesthesiologists until the 1990's. At that time descriptions of placement for breast surgery and thoracotomy cases were published, but did not lead to its widespread adoption. The TPVB could be considered to be largely forgotten and underutilized by anesthesiologists.1 In 1992 Lonnqvist reported the classic approach in children. Very little was published between 1999 and 2009 when ultrasound approaches were first described. Since 2009 the TPVB has experienced a brisk resurgence with new approaches and indications likely due to the flexibility of ultrasound guided placement. There are now many good trials and case series showing its benefit in upper abdominal, breast, thoracic, and flank incisions, and even a review of studies using bilateral placement.2 Widespread implementation for accepted indications appears to remain low.
Technical Approaches:
The major difference in performance techniques can be summarized as landmark-based vs. ultrasound guided (USG). Ultrasound imaging is used to approach the paravertebral space in different ways, and no one way enjoys a dominant practice in the literature. Commonly described technical approaches for single shot and catheter placement include:
- Landmark sagittal with needle perpendicular to the skin walking superiorly off and 1-1.5 cm deep to the transverse process which may be combined with loss of resistance, nerve stimulation, or calculated depth as using the formula 10.2 + (0.12 x weight in kilograms).3, 12 Figures 1A, 1B.
- USG sagittal out-of-plane lateral to medial. In this first description of an USG technique, indentation of the pleura with injection was noted to be confirmatory.4 Figures 2A, 2B.
- USG sagittal in-plane inferior to superior. Proponents of this approach note steep angle, and pleura indentation with injection.5 Figures 2A, 2B.
- USG transverse in-plane lateral to medial placement with an oblique intercostal probe orientation. The ability to visualize the needle until it passes under the transverse process makes this a very attractive approach for infants and children.6 Figures 3A, 3B.
- USG transverse out-of-plane immediately lateral to the transverse process.7 Figures 3A, 3B.
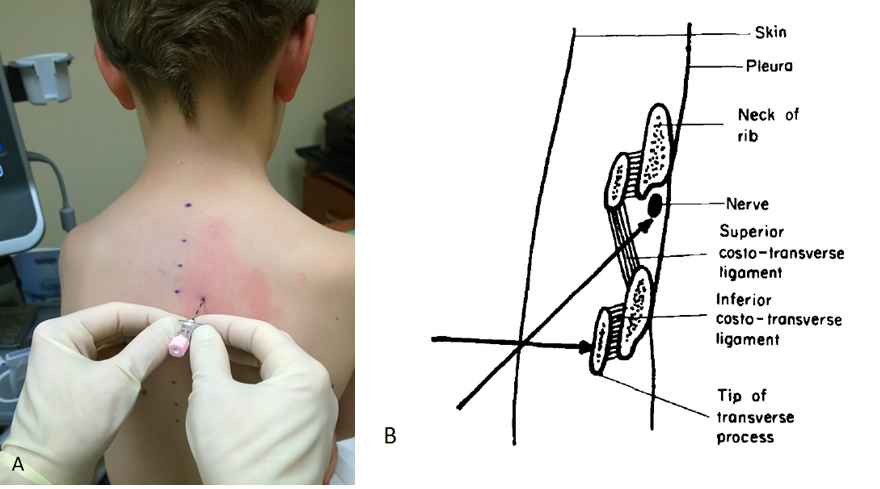
Figure 1A Landmark sagittal approach 2 cm lateral to spinous process with skin entry and depth estimated by USG. Figure 1B Recommendation for caudal to cranial needle direction based on perpendicular piecing of the superior costo-transverse ligament when needle is walked superiorly off the tip of the TP.1 Permission to reprint figure granted by publisher.
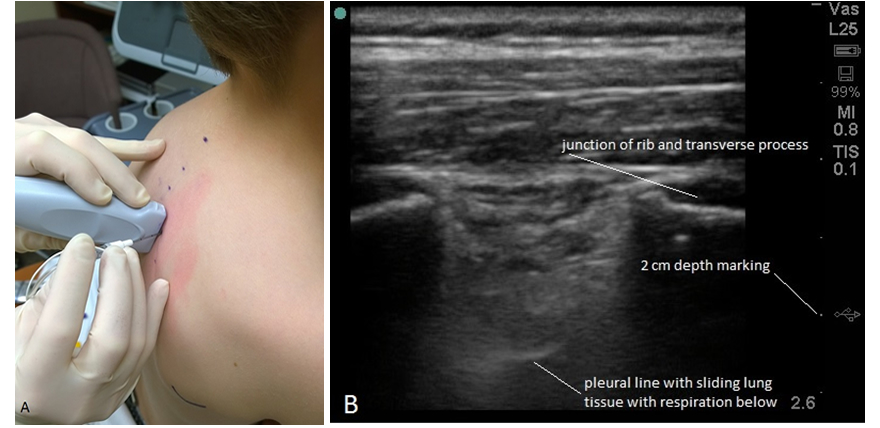
Figure 2A Probe positioning for the USG sagittal out-of-plane approach. Figure 2B Ultrasound view in the sagittal plane approximately 2 cm lateral to midline.
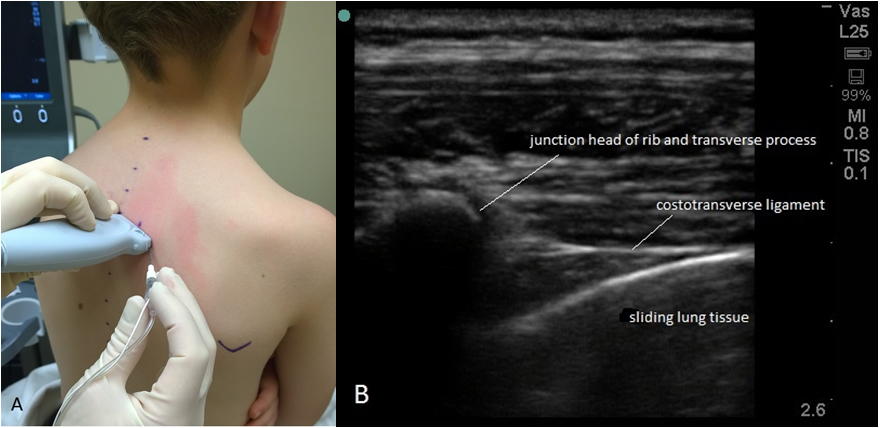
Figure 3A Probe positioning and needle direction for the USG transverse in-plane approach. With the USG transverse out-of-plane approach, the needle would be placed inferior to the midpoint of the probe. Figure 3B Transverse oblique intercostal ultrasound view.
NOTE: All photos were taken with the assent of my 8 year old son, who was rewarded for his effort with a trip to his favorite restaurant. Simulated needling with gloved hands and unsterile probe using B. Braun PERIFIX® 18 guage x 5 cm Tuohy epidural needle and a Life-Tech, Inc. ProLong® 19 guage x 5 cm block needle. Both needles were modified for photograph by breaking off distal 2 cm to simulate estimated depth of insertion if it had been a real block performance.
Recent pediatric studies seem to favor the USG transverse in-plane approach.8 However, a recent trial of 60 infants undergoing cardiac thoracotomy comparing epidural and TPVB infusions showed equal efficacy and reduced side effects and failures using the landmark technique calculating depth of needle insertion in millimeters as 10.2 + (0.12 x weight in kilograms) with no incidence of failed placement.9 The landmark technique may be a faster technique in highly skilled hands, but the ultrasound guided approaches are very attractive in teaching settings where blind needling can be stressful for the teacher and student.
We recently presented a case report where we utilized a modified approach for a successful paravertebral catheter placement in a patient with severe (80 degree curvature) scoliosis and an intrathecal baclofen pump who was undergoing upper abdominal surgery with unilateral incision. We utilized ultrasound to scan the anatomy from numerous angles and planes and to develop a "mental picture" of her unique paravertebral space on the convex side. Subsequently, the needle was inserted without ultrasound guidance, walking off the dysmorphic transverse process resulting in a successful catheter placement.10 See Figure 4A and 4B.
"Denting of the pleura" with saline or local anesthetic injection is often advised to confirm correct placement in the paravertebral space. Absence of pleural denting does not indicate failure of needle placement, and is best considered a confirmatory sign. As with thoracic epidural placement, contrast radiography is the most accurate of all confirmatory methods because it accurately reveals level, spread, and can readily identify epidural, vascular, spinal, or pleural misplacement.
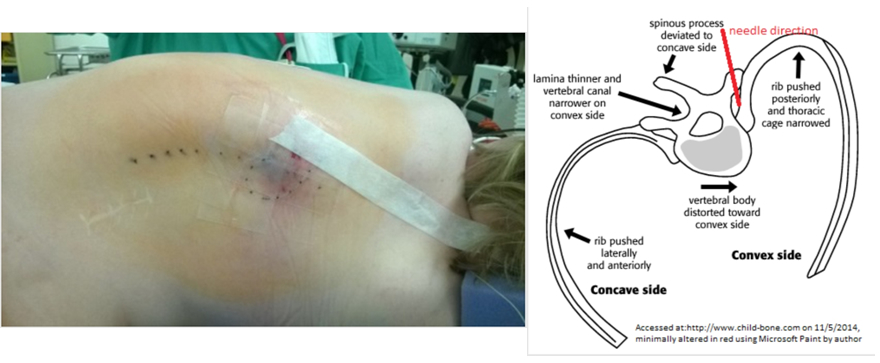
Figure 4A Patient positioning with spinous processes marked, and catheter secured.10 Figure 4B Needle direction of block approach in this patient.10
Advantages/benefits:
Compared to thoracic epidural analgesia (TEA), the TPVB catheter infusions have a lower incidence of side effects such as pruritus, urinary retention, hypotension, and lower extremity weakness.9 When used as part of a postoperative regiment, TPVB can facilitate chest tube tolerance with little additional opioids or sedatives in children. Epidural catheters may be removed between day 2-3 whereas TPVB catheters are commonly continued until chest tubes are removed, which is typically 3-6 days postoperatively.
Limitations/risks:
Objections by anesthesiologists to performing catheter placement are often those of convenience. Either a skilled regional anesthetist is not available to perform the procedure, or is reluctant to discuss new indications with surgeons who are generally more familiar with an opioid PCA for postoperative pain control. When used for post-thoracotomy pain control, continuous nerve blocks need to be managed over several days in a collaborative environment as part of an acute pain service, and this can be time consuming. Moreover, it may not be reimbursed commensurate to the effort expended, at least not during startup of a regional anesthesia service. However, with effective communication, collaboration and persistence, the TPVB can become an effective and appreciated method of pain control by intensivists, surgeons, nursing staff, and families.
Anticoagulation may be less of a risk factor when performing a paravertebral block which does not contain as high a concentration of vascular structures as the neuraxis, and in not a pressure limited space like the epidural canal. Limited case reports, and lack of recommendations for this indication suggest caution when considering placement of this block in an anticoagulated patient.
Duration of safe infusion is an area of continuing debate. As nerves are blocked somewhere between a neuraxial and peripheral location, the duration of infusion could range between 3-7 days. Older case series of surgeon-placed TPVB catheters are reported to have been routinely run for five days.11 It may be prudent to accept a practice of catheter infusion duration somewhere between that recommended for the epidural and peripheral nerve catheter infusions; perhaps five days is a safe upper limit until studies of plasma levels of local anesthetic at longer intervals indicate a lower level of concern. Our practice is to continue TPVB infusion for up to five days in infants and children. Neonates receive 1.5% cholorprocaine infusions similar to neonatal epidural infusion practice, and older children may receive Ropivacaine 0.15% infusions although other solutions are not precluded.
Summary:
TPVB with catheter infusion has been used for over a century for painful conditions of the thoracic wall. Recent resurgence of interest is attributed to USG placement techniques. It is too soon to recommend one technique of insertion as superior to another. Similar to endotracheal tube placement techniques, it would be good for the practitioner to develop a number of placement approaches using what works best in their setting. Described local anesthetic concentration and duration of infusion are highly variable. Future reports from large databases such as the Pediatric Regional Anesthesia Network (PRAN) may help refine recommended techniques and management. However, local implementation of the TPVB need not wait for large scale acceptance. It is the author's opinion that whenever possible, TPVB infusions should be routinely used for unilateral thoracotomy surgery, to facilitate tolerance to large bore chest tube drainage, and for unilateral rib fracture analgesia.
References:
- Eason MJ, Wyatt R. Paravertebral thoracic block - a reappraisal. Anaesth 1979; 34:638-642
- Richardson J, Lonnqvist PA, Naja Z. Bilateral thoracic paravertebral block: potential and practice. British J of Anaesth 2011; 106:164-171
- Lonnqvist PA. Continuous paravertebral block in children initial experience. Anaesth 1992; 47: 607-609
- Hara K, Sakura S, Nomura T, Saito Y. Correspondance: Ultrasound guided thoracic paravertebral block in breast surgery. Anaesth 2009; 64:216-229
- O Riain S, Donnell BO, Cuffe T, Harmon DC, Fraher JP, Shorten G. Thoracic paravertebral block using real-time ultrasound guidance. Anesth Analg 2010; 110:248-251
- Renes SH, Bruhn J, Gielen MJ, Scheffer GJ, van Geffen GJ. In-plane ultrasound-guided thoracic paravertebral block. A preliminary report of 36 cases with radiologic confirmation of catheter position. Reg Anesth Pain Med 2010; 35:212-216
- Marhofer P, Kettner SC, Hajbok L, Dubsky P, Fleischmann E. Lateral ultrasound-guided paravertebral blockade: an anatomical-based description of a new technique. British J of Anaesth 2010; 105:526-532
- Boretsky K, Visoiu M, Bigeleisen P. Ultrasound-guided approach to the paravertebral space for catheter insertion in infants and children. Pediatr Anesth 2013; 23:1193-1198
- El-Morsy GZ, El-Deeb A, El-Desouky T, Elsharkawy AA, Elgamal MAF. Can thoracic paravertebral block replace thoracic epidural block in pediatric cardiac surgery? A randomized blinded study. Ann Cardiac Anaesth 2012; 15:259-253
- Longanecker J, Thompson ME. Ultrasound-guided continuous thoracic parabertebral block in a pediatric patient with severe scoliosis and an intrathecal baclofen pump undergoing major abdominal surgery. Abstract presented at the fall ASRAPM meeting November 2014 San Francisco
- Eng J, Sabanathan S. Continuous paravertebral block for post-thoracotomy analgesia in children. J Paediatr Surg 1992; 27:556-557
- Lonnqvist PA, Hesser U. Depth from the skin to the thoracic paravertebral space in infants and children. Pediatr Anesth 1994; 4:99-11