Cosyntropin for Use in Treatment of Post-Dural Puncture Headaches in Pediatric Patients
By Priscilla J. Garcia, MD, Angela Medellin, Brady Moffett, Shireen Hayatghaibi, Kim P. Nguyen, MD
Texas Children's Hospital, Baylor College of Medicine, Houston, TX, USA
(Summarized and submitted by Priscilla J. Garcia, MD)
Post-dural puncture headache (PDPH) is the most common complication after a lumbar puncture (LP) (Ona, 2013). Treatment for PDPH consists of both conservative and invasive modalities. Conservative treatment includes hydration, nonsteroidal anti-inflammatory drugs (NSAIDS), caffeine, and anti-emetics. While invasive, autologous epidural blood patch (EBP) is considered the definitive treatment for PDPH. Complications include radicular pain from nerve root irritation or displacement, cranial nerve palsies, meningeal irritation, elevated intracranial pressure, paresthesias, cauda equine syndrome, infection, back pain, and subdural hematomas. Contraindications include patient refusal, fever or suspected bacteremia, and anticoagulation (Frank, 2006). Though not an absolute contraindication, there is significant hesitation to administer autologous blood for EBP in patients diagnosed with leukemia (Bucklin, 1999).
Another option involves administration of cosyntropin, an ACTH analog. Cosyntropin increases the production of CSF by stimulating the release of aldosterone, thus decreasing the amount of traction and producing mild beta-endorphin effects (Zeger, 2012). While an adult study demonstrated reduction of PDPH with cosyntropin prophylaxis (Hakim, 2010), there are no pediatric studies that examine its efficacy. The purpose of this study was to compare the efficacy of cosyntropin versus invasive treatment in the pediatric population at a tertiary hospital.
This study was an IRB-approved retrospective cohort review. Patients who experienced PDPH were identified from the EMR system for a time period of seven years, October 2010 – June 2017. Patient groups included subjects that received a conservative treatment regimen for PDPH, patients who received EBP, and patients who received cosyntropin. Data collected for each groups included: patient age, weight, ASA status, medications and dose administered, fluid administration, if EBP performed, and medical history. Minitab software (version 17; Minitab Inc, State College, PA) was used to calculate descriptive statistics. Patient characteristics across treatment groups were compared using the students' t-test.
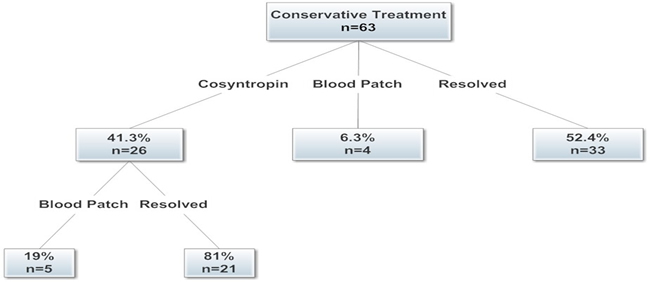
A total of 63 patient’s presented with PDPH (41 females and 22 males) during the study timeframe (age range: 5 years – 21 years, mean: 14 years). Patient characteristics by group were analyzed to assess for differences. ASA status was the only variable in demographics that differed between groups. All patients included in the study received conservative treatment of IVFs and caffeine. Of these, 52.4% (n=33/63) of these patients experienced resolution with conservative treatment alone, while 6.3% (n=4/63) received a blood patch after conservative treatment failed to provide full resolution of symptoms. 41.3% (n=26/63) received cosyntropin after conservative treatment failed to provide resolution of symptoms of which 81% (n=21/26) experienced resolved symptoms. Only 19% (n=5/26) continued on to EBP after receiving cosyntropin. Currently, there are no pediatric dosing guidelines for the use of cosyntropin for PDPH. Cosyntropin was administered at a dose of 1 mg in 22/26 patients, and 4/26 patients were administered a dose of 0.5 mg. Doses given were based on patient body weight.
Our study demonstrates that cosyntropin is an effective option for treating PDPH. Cosyntropin can be used as a secondary treatment option after other conservative treatment fails, avoiding the performance of an invasive EBP procedure and anesthetic in pediatric patients.
Figure 1: Patient characteristics.
*Control group includes patients with EBP and those whose symptoms resolved after conservative treatment
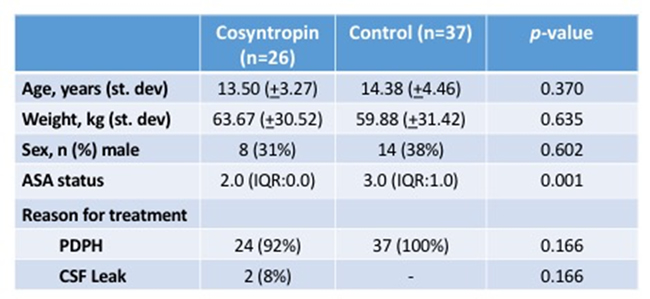
Figure 2: Treatment flowchart
References:
- Bucklin BA et al. “Clinical dilemma: a patient with postdural puncture headache and acute leukemia.” Anesth Analg 1999; 88: 166-7.
- Frank RL et al. “Lumbar puncture and post-dural puncture headaches: implications for the emergency physician.” J of Emergency Med 2006; 35: 149-157.
- Hakim SM. “Cosyntropin for prophylaxis against postdural headache after accidental dural puncture.” Anesthesiology 2010; 113:413-20.
- Ona X B et al. “Drug therapy for preventing post-dural puncture headache” Cochrane Database of Systematic Review 2013: issue 2: art. No.: CD001792.
- Zeger W et al. “Comparison of cosyntropin versus caffeine for post-dural puncture headaches: a randomized double-blind trial. World J Emerg Med 2012; 3(3): 182-185.