Erector Spinae Plane Catheters for Pain Management of Rib Cartilage Harvesting for Stage 1 Microtia Reconstruction: A Retrospective Study
By Carole Lin, MD and Curtis Darling, MD
Department of Anesthesia, Lucile Packard Children’s Hospital at Stanford; Stanford University School of Medicine, Stanford, California
(Summarized and submitted by Carole Lin, MD)
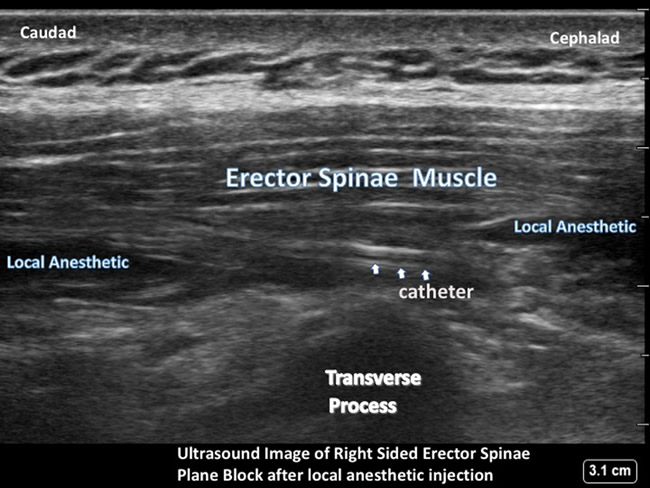
The erector spinae plane (ESP) block is a regional technique that was first described as a technique for the intervention of neuropathic pain in 2016.1 It is a novel ultrasound-guided inter-fascial plane block that involves administration of local anesthetic agents, adjuncts, and/or catheters into the fascial plane under a composite of paraspinal muscles (Iliocostalis, Longissimus, Spinalis) known collectively as the erector spinae muscles. While the exact mechanism of action of the block is presently unknown, it has been used as an analgesic technique with applications ranging from neck and shoulder surgery, thoracic, abdominal, and hip surgery.3-5
Microtia is a congenital deformity characterized by the underdevelopment or lack of an external ear. Microtia repair addresses the reconstruction of a hypoplastic or absent ear in two stages. The first stage involves harvesting the rib cartilage from the chest and then this cartilage is sculpted on a framework to the likeness of the opposite ear. The second and subsequent surgical operations involve lifting the posterior ear, improving the shape of the ear, or removing scars. The age of repair is typically 8-10 years old, when the social and psychological impact of the congenital deformity is impactful to their lives. By this time, patients can be more mature and motivated to undergo the procedure. This repair can be done any age, and there are adult patients who request this surgery as well.
The challenge of pain management for patients undergoing a stage 1 microtia reconstruction is primarily the rib cartilage harvest site. The site of ear reconstruction is generally not a significant source of pain. Chest wall pain, improperly managed, can lead to compromised breathing and movement, thus complicating the recovery of patients with issues of hypoxemia, atelectasis, delay or inability to meet physical therapy goals, and delayed discharge. New literature has introduced a novel method for treating painful rib pathology with the erector spinae plane catheter with more studies and case reports supporting safety and efficacy of the technique. Current options for pain control include a thoracic epidural, intrathecal morphine, intravenous or oral narcotics and adjuncts, and a local anesthetic infusion catheter at the incision site attached to an On-Q pump. Presently, the standard at our institution is the On-Q catheter which, while effective when properly working, has demonstrated some inconsistencies with effective pain control. After the rib cartilage graft is harvested, the surgical team places a multiport catheter above the closed muscle and below the serosal closure. This catheter is connected to the On-Q pump system. The On-Q pump system is an elastomeric pump which allows delivery of a local anesthetic at a set rate to the site.
We propose the ESP block produces a more consistent multi-dermatomal sensory block. Anatomical and radiological investigation in fresh cadavers and MRI contrast dye studies indicate that its likely site of action is at the dorsal and ventral rami of the thoracic spinal nerves.2 The ESP block produces additional intercostal spread, which may contribute to more extensive analgesia. This additional spread is important because the rib graft harvesting is typically done on the same side as the ear reconstruction and depending on the size of the construct may be 2-3 levels (T-9-11) of cartilage removal.
In a preliminary analysis, we retrospectively reviewed five patients who received erector spinae plane catheters from January 2018 to March 2018. The ESP catheter was used in five patients over a period of two months with no patient exclusions. The age range of the patients were 7-47 years with a mean of 17.6 years. The mean pain scores for day 1 through 4 are shown on table 1.
Table 1.
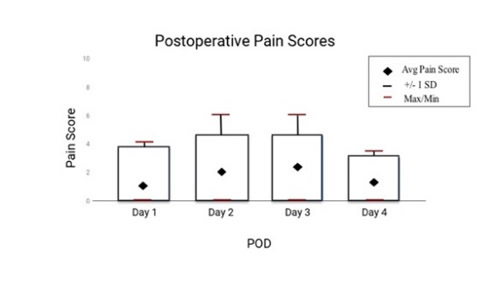
Pain scores were highest on days 2 and 3 with a decrease in pain by day 4. During the first 24 hours, patients received around-the-clock nonsteroidal anti-inflammatory drugs (NSAIDs), low-doses of background hydromorphone as prn doses, and minimal adjustments to the ESP catheter infusion rates. Four out of five patients transitioned to oral pain management by POD day 2. One patient did report consistently higher pain scores than other patients, however, total narcotic use was consistent with the others. Another patient had nausea associated with hydromorphone and was transitioned to nalbuphine with resolution of nausea. The patients receiving ESP catheters demonstrated less opioid use while the catheter remained in place. In one patient, the ESP catheter was removed after 15 hours of use and was transitioned to oral oxycodone, with the total amount of required opioids was noted to be higher after the ESP was pulled. There were no infections, local anesthetic systemic toxicity, and no complications from the ESP catheter on postoperative follow up.
This retrospective review introduces the ESP catheter as a reliable adjunct in a multimodal approach to pain management for rib graft harvesting in stage 1 microtia reconstruction. Our experience with five patients suggests that the ESP catheter can provide a level of analgesia allowing for decreased IV and PO opioid use postoperatively. Clinically, patients reported minimal to no pain when they were not actively moving. Higher pain scores were during movement on the first two days and underscores the importance of as-needed analgesic dosing prior to activity such as physical therapy. Our experience with the ESP catheter suggests that the analgesic expectations of the block should not be the same as those seen with dense neuraxial or peripheral nerve blocks. In contrast, the ESP and other inter-fascial plane blocks should be considered as another tool in a multimodal approach to pain management. A retrospective analysis comparing the On-Q and ESP catheters for use in postoperative pain management in stage 1 microtia rib harvesting is ongoing. Additionally, a randomized prospective study comparing the two institutional techniques is also in development.

References:
- Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The Erector Spinae Plane Block: A Novel Analgesic Technique in Thoracic Neuropathic Pain. Reg Anesth Pain Med. 2016 Sep-Oct;41(5):621-7.
- Adhikary, Sanjib Das, MD; Bernard, Stephanie, MD; Lopez, Hector, MD; Chin, Ki Jinn, FRCPC. Erector Spinae Plane Block Versus Retrolaminar Block: A Magnetic Resonance Imaging and Anatomical Study. Regional Anesthesia and Pain Medicine: May 23, 2018 - Volume Online First - Issue - p
- Hernandez MA, Palazzi L, Lapalma J, Forero M, Chin KJ. Erector Spinae Plane Block for Surgery of the Posterior Thoracic Wall in a Pediatric Patient. Reg Anesth Pain Med. 2018 Feb;43(2):217-219.
- Adhikary SD, Pruett A, Forero M, Thiruvenkatarajan V. Erector spinae plane block as an alternative to epidural analgesia for post-operative analgesia following video-assisted thoracoscopic surgery: A case study and a literature review on the spread of local anaesthetic in the erector spinae plane. Indian J Anaesth. 2018 Jan;62(1):75-78.
- Hernandez MA, Palazzi L, Lapalma J, Forero M, Chin KJ. Erector Spinae Plane Block for Surgery of the Posterior Thoracic Wall in a Pediatric Patient. Reg Anesth Pain Med. 2018 Feb;43(2):217-219.