Opioid Stewardship
By De-An Zhang, MD1, Eric McCoy, MD2, Cynthia Nguyen, MD1, Robert Cho, MD1, Selina Poon, MD1
1Shriners for Children Medical Center, Pasadena, CA, USA,
2Harbor-UCLA Medical Center, Torrance, CA, USA
(Summarized and submitted by De-An Zhang, MD)
Management of acute surgical pain with opioid analgesia carries risk of future nonmedical use, with studies finding patients who are prescribed opioid analgesics for acute surgical pain have a 3% to 10% increased risk of becoming opioid dependent.1-3 Residual opioids from previous legitimate prescription may be a gateway to opioid diversion and abuse, especially when adolescents reside in the home.4
In 2016, we began asking our patients to record the amount of opioids consumed following surgery as part of our opioid stewardship program. From June 2016 through April 2018, we collected 277 patient reported outcomes for outpatient hand, plastic, and orthopedic surgery. Of all opioid doses prescribed, 89.2% went unused. Over half of the patients, (n = 143, 52%) did not use any opioid medications post-operatively. For the subset that used opioids (n=134) during the acute post-operative period, an average of 3.8 ± 4 doses were used over an average of 2.4 ± 1.7 days. Figure 1 is a histogram representing the number of doses taken per patient.
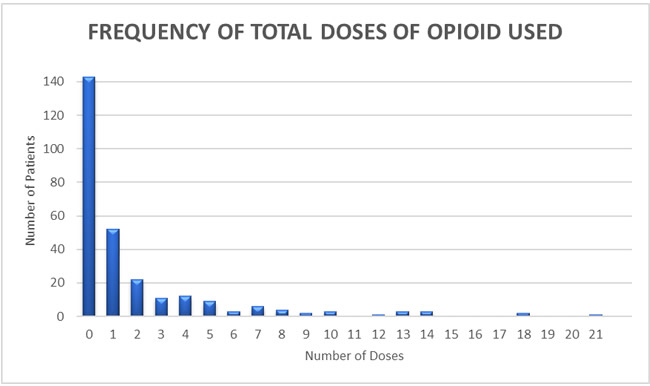
Figure 1: The majority of patients (52%) used 0 doses of opioid. A prescription of 9 doses would cover 90% of patients while a prescription of 13 doses would cover 95% of all patients.
We then compared the opioid usage of patients who had surgery that involved manipulation of bone versus soft tissue only. As expected, patients that underwent bone surgery were more likely to use an opioid (55.2% vs 40.9%, p = 0.022). However, when looking at the subset of patients that used opioids, there was no significant difference in amount used (3.8 ± 4 vs 3.9 ±4.1, p = 0.994) or in the duration (2.3 ± 1.7 vs 2.5 ± 1.8, p = 0.677) of usage for patients who underwent bone versus soft tissue surgery. With an understanding that most of opioids prescribed were unused, we began asking our patients if they knew how to properly dispose of their unused opioids. From February to August of 2018, 102 patients were interviewed. Only 15 patients (14.7%), knew how to properly dispose of their opioids prior to their visit; the majority of whom (9) cited the flushing medications down the toilet as their known method (as recommended by the FDA). The only demographic variable correlated with knowledge was English as the primary language spoken at home.
Following outpatient surgery, many patients are prescribed opioids for post-operative pain. Our data suggests that most patients are prescribed more doses than are needed. As a practice, we have limited our outpatients to 10 doses of opioids post-operatively. Furthermore, most of our patients, especially the non-English speakers, do not properly know how to dispose of their leftover opioids. Our medical center is making plans to not only educate all our patients, but to provide them, cost-free, an FDA approved take-home disposal product.
References
- Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014 Feb 11;348:g1251. doi:10.1136/bmj.g1251. PubMed PMID: 24519537; PubMed Central PMCID: PMC3921439.
- Brummett CM, Waljee JF, Goesling J, Moser S, Lin P, Englesbe MJ, Bohnert ASB, Kheterpal S, Nallamothu BK. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA Surg. 2017 Jun 21;152(6):e170504. doi: 10.1001/jamasurg.2017.0504. Epub 2017 Jun 21. PubMed PMID: 28403427.
- Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med. 2012;172(5):425-430.
- McCabe SE, West BT, Veliz P, McCabe VV, Stoddard SA, Boyd CJ. Trends in Medical and Nonmedical Use of Prescription Opioids Among US Adolescents: 1976-2015. Pediatrics. 2017 Apr;139(4). pii: e20162387. doi: 10.1542/peds.2016-2387. Epub 2017 Mar
- PubMed PMID: 28320868; PubMed Central PMCID: PMC5369669.