Local Anesthetic Systemic Toxicity Update
By Mauricio Arce Villalobos, MD; Tarun Bhalla, MD, MBA, FAAP; Joseph D. Tobias, MD, FAAP
Department of Anesthesiology & Pain Medicine
Nationwide Children’s Hospital; The Ohio State University
Columbus, Ohio
Over the recent decades, there have been significant advances in regional anesthesia techniques and equipment, resulting in the increased use of these techniques in surgical procedures worldwide.1 Pediatric regional anesthesia has become an integral component of the perioperative anesthetic plan. Unlike the adult population, where both neuraxial and peripheral nerve blockade are performed in awake patients, thereby providing a "monitor" to potentially reduce adverse effects in these interventions, these techniques are generally and routinely performed under deep sedation or general anesthesia in pediatric patients.2
The incidence of complications related to regional anesthesia in infants and children remains extremely low, with a reported incidence of transient neurological deficits in 2.4 cases per 10,000 and local anesthetic systemic toxicity (LAST) in 0.76 cases per 10,000 procedures.3 However, whenever an intervention of this nature is to be performed, regardless of whether it is a pediatric or adult patient, the practitioner must be aware of possible complications, means for early identification, and more importantly, overall management to prevent severe sequelae or death.
Treatment of toxicity related to local anesthetics agents (LAAs) extends beyond the arena of anesthesiology as these agents are used during a variety of procedures in the field of medicine and surgery, outside of the operating room, in the emergency department in both inpatients and outpatients. LAAs are used with high frequency in pediatrics to provide anesthesia or regional analgesia by various routes. Regardless of the route of administration, systemic absorption is a possibility, and if high plasma concentrations are achieved, systemic toxicity may occur. There can be a disruption of action potentials within the central nervous system (CNS) as well as in the cardiac conduction system. This occurs from reversible blockade of voltage dependent sodium channels, which inhibits the flow of ions through the cell membrane.
At the level of the CNS, LAAs will express their toxicity by two mechanisms including both excitatory (activation) and inhibitory (suppression) pathways mediated by N-methyl-D-aspartate (NMDA) and aminobutyric acid (GABA) receptors, respectively. These interactions are responsible for the genesis of clinical manifestations ranging from taste alterations and circumoral numbness to seizures. As the concentration of the LAA continues to increase, an inhibitory effect is produced in the aforementioned excitatory pathways, leading to the creation of an electrical silence in the electroencephalogram, clinically manifesting as coma and respiratory arrest.4
Cardiotoxicity has two forms of presentation: arrhythmias and myocardial depression. The spectrum of arrhythmias is variable including bradyarrhythmias, reentry tachyarrhythmias, wide complex arrhythmias, and cardiac arrest. At the myocardial level, the blockade of the sodium and potassium channels leads to reentry arrhythmias due to disruption of the intrinsic conduction system.5 The degree of sodium channel block by LAAs is dependent upon the state of that channel as LAAs have a high affinity for channels in the open or inactivated states and a low affinity for channels in the rested state. Consequently, block of sodium channels develops during the upstroke and plateau of the action potential and dissipates during the diastolic interval. By prolonging the depolarization phase, the affinity for the channels is increased, thus prolonging the presence of the LAA molecules in the myocardium and therefore its clinical effects.6
Because the structure of the voltage-dependent calcium channels closely resembles that of the sodium channels, LAAs block these channels by the same mechanism. Calcium channels are extremely important in synaptic transmission and within cardiac muscle cells where they are involved in the coupling of electrical excitability with mechanical contraction.7 These effects can cause myocardial depression, leading to a decrease in intracellular calcium release by the sarcoplasmic reticulum, and therefore decreasing contractility. In addition, there is an inhibitory phenomenon with inactivation of β-adrenergic receptors and depressed adenylate cyclase activity resulting in decreased generation of cyclic AMP.8 Bupivacaine can also accumulate in the mitochondria of metabolically active tissue and uncouple oxidative phosphorylation thereby decreasing ATP synthesis. The reduction in ATP production at this level results from decreased fatty-acid oxidation because LAAs block fatty-acid transport into the mitochondria by inhibiting carnitine acylcarnitine translocase (CACT). All of these effects are exacerbated during hypoxemia and hypercarbia.9
The spectrum of clinical presentation can vary significantly. According to published reports; CNS manifestations occur 43% of the time, CV manifestations occur 24% of the time, and a combination of both CNS and CV occur in 33% of the cases.13 In the case of many pediatric patients, CV symptoms are the primary manifestations during procedures, as the patient may be receiving general anesthesia or sedation.
As LAST occurs when the plasma concentration of the LAA exceeds the toxic threshold, it is imperative to not exceed the maximum dose recommendations for a specific LA by either bolus dosing or continuous infusions. Various comorbid conditions may affect the pharmacokinetics of LAAs and must be considered on a case-by-case scenario when dosing considerations are made. Patient-related conditions may have a direct influence on systemic uptake, metabolism, and toxicity of LAAs. In newborns, the levels of α-glycoprotein acid (AAG), which binds LAAs, are 50% lower than the values of an adult, suggesting higher risk of increase in their plasmatic levels. In renal dysfunction and uremia, clearance of LAAs has been shown to be decreased in comparison to nonuremic patients, on the other hand, there is an increase in AAG which bounds to LAAs thus offering an important protection mechanism by decreasing the amount of unbound compounds that can cause LAST.
The hyperdynamic state which is associated with renal failure anemia contribute to a rapid rise in the plasma concentration of LAAs after their injection by promoting their rapid absorption.10 Heart failure or conditions associated with decreased cardiac output increase the risk of LAST by reducing hepatic perfusion thus metabolism and clearance of LAAs is decreased. Hepatic failure, not only decreased the metabolism of many LAAs, but is associated with lower levels of plasma proteins that bind LAAs thereby increasing the free or unbound fraction thus increasing the risk of LAST.11 The vascularity, tissue binding properties, and presence of vasoconstrictors (epinephrine) will influence the absorption of LAAs from the tissues into the circulation. The blood level of LAAs depends on the total dose administered and is independent of the concentration of the injected solution (no difference with a 0.5% or a 0.25% solution). The plasma concentration is also dependent on the vascularity of the site of injection, being highest for intercostal and interpleural sites and lowest for subcutaneous and peripheral nerve blockade.12
To reduce the incidence of LAST, prevention is of primary importance. The most important aspect in prevention is meticulous attention to dosing related to both single injections and the administration of continuous infusions. No intervention in isolation will eliminate risk, it is a multifactorial process. According to the most recent ASRA practice advisory, there are three factors that are fundamental in prevention14:
- avoid or recognize the intravascular injections of LAAs
- mitigate the systemic absorption
- awareness of patients that are at greater risk
In regard to point #3, the ASRA 2017 practice advisory focuses on three things in particular. LAAs are usually stored in skeletal muscle, thus patients with low muscle mass are at higher risk for LAST and these patients may be at the extremes of ages. Secondly, anesthesiologists may use “safer” LAAs in comparison to the traditional bupivacaine; however, these agents still have the potential to cause LAST. Safety measures should be upheld at all-times regardless of the LAA that is used. Finally, approximately 15% of LAST episodes involve continuous infusions, usually between 1-4 days after initiation and their clinical presentation is subtle.10
Routine use of ultrasound has decreased the incidence of vascular puncture associated with peripheral nerve blockade. When compared with landmark techniques, ultrasound has reduced LAST episodes by 65%.15 The use of a test dose (0.1 mL/kg of a solution containing 1:200,000 epinephrine) has been used frequently in the practice of pediatric regional anesthesia to assess accidental intravascular injection. According to the most recent ESRA-ASRA guidelines, the use of test dose in all experimental studies using deliberate IV injection of this solution resulted in no false-positive results. Thus, any change in the T wave of the ECG or increase in the heart rate by 10 beats/min within 30-90 seconds after injections should be considered an inadvertent IV injection until proven otherwise.2
While the safety of regional anesthesia and the incidence of LAST has decreased in the practice of pediatric anesthesia, our medical and surgical colleagues frequently use LAAs. In a recent review of case reports of LAST episodes, penile blocks accounted for 23% being followed by local infiltration analgesia (17%). Of the total episodes reported, 49% were performed by anesthesiologists while the other 51% by surgeons, dentists, emergency medicine physicians, and pediatricians. Given this information, guidelines, policies, and education regarding LAST should include our non-anesthesia colleagues.
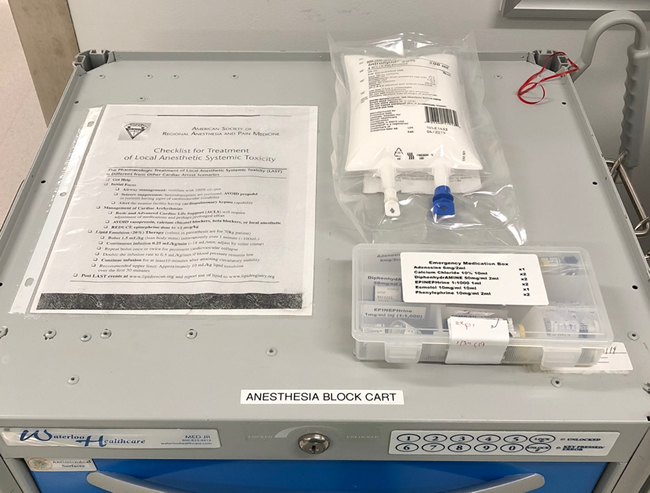
Treatment of LAST episodes initially focuses on securing the airway thus preventing hypoxia, hypercarbia and acidosis, factors that enhance the severity of LAST and negatively affect resuscitation. After appropriate resuscitation efforts have been initiated, the first line of management from a pharmacological point of view is lipid emulsion therapy. Early initiation of effective CPR is important to ensure that coronary perfusion is preserved thus helping reduce LAAs myocardial concentrations and attain maximum benefit from lipid emulsion therapy. Use of epinephrine at doses of 1 ug/kg or less, remains fundamental in the management of hemodynamic collapse that doesn’t respond to lipid emulsion therapy. Use of the ASRA checklist has proven effective when used in simulations and helps the operator to follow the current recommendations in an appropriate manner.16 As such, these guidelines and intralipid should be readily available whenever LAs are used. (Figure 1)
Figure 1. Anesthesia block cart with ASRA checklist, Intralipid 20%, and emergency medication box.
Lipid emulsion therapy was proposed for the management of LAST for the first time in 1998 and was accepted in clinical practice years later. There are many proposed mechanisms of action, the most prominent involve the hypothesis that lipid emulsion create an intravascular lipophilic sink into which lipid soluble LAAs are partitioned and thereby removed from the active circulation and tissues. Nowadays, lipid emulsion therapy is believed to involve multiple mechanisms summarized in three specific effects.17 The first includes a shuttling effect, in which the lipid molecules act as dynamic transporters of LAA molecules out of the highly perfused organs with redistribution to organs that store and metabolize the drug. Second, is a direct cardiotonic effect on cardiac muscle, with increased contractility and improvement of cardiac output and blood flow.
Finally, LAAs activate multiple cellular apoptotic pathways in cardiac cells which are blocked or reversed by lipid emulsion therapy.
Current recommendations for the treatment of LAST include:14
- Prompt and effective management of the airway thus preventing hypoxia, hypercarbia, and acidosis.
- Lipid emulsion therapy
- 20% lipid emulsion bolus (initial)
- 100 mL over 2-3 minutes if the patient is over 70 kg
- 1.5 mL/kg over 2-3 minutes if the patient less than 70 kg
- 20% lipid emulsion infusion
- 200-250 mL over 15-20 minutes if the patient weighs more than 70 kg
- 0.25 mL/kg/min if patient weighs less than 70 kg
- Continue infusion for a minimum of 10 minutes after return to spontaneous circulation.
- 12 mL/kg is recommended as the upper limit for initial dose
- Avoid using propofol
- Seizure control with benzodiazepines, if seizures persist, use NMBA to reduce hypoxemia and acidosis
- If cardiac arrest occurs
- Use epinephrine (less than 1 ug/kg)
- Avoid calcium channel blockers and β-adrenergic receptor antagonists.
- Amiodarone is preferable if ventricular arrhythmias develop.
- Failure to respond to all previous efforts should prompt institution of cardiopulmonary bypass or extracorporeal membrane oxygenation (ECMO).
References
- Lam DK, Corry GN, Tsui BC. Evidence for the use of ultrasound imaging in pediatric regional anesthesia: a systematic review. Reg Anesth and Pain Med 2016; 41:229-41.
- Ivani G, Suresh S, Ecoffey C, et al, The European Society of Regional Anesthesia and Pain Medicine and the American Society of Regional Anesthesia and Pain Medicine joint committee practice advisory on controversial topics in pediatric regional anesthesia. Reg Anesth and Pain Med 2015; 40:526-532
- Walker BJ, Long JB, Sathyamoorthy M, et al, Complications in pediatric regional anesthesia, An analysis of more than 100000 blocks for the pediatric regional anesthesia network. Anesthesiology 2018; 129: 721-732
- Sugimoto M, Uchida I, Fukami S, et al, The alpha and gamma subunit-dependent effects of local anesthetics on recombinant GABA receptors. Eur J Pharmacol 2000; 401:329–37.
- Groban L, Central nervous system and cardiac effects from long-acting amide local anesthetic toxicity in the intact animal model. Reg Anesth Pain Med 2003; 28:3–11.
- Tasch M, Butterworth J. Toxicity of local anesthetics.ASA Refresher Courses in Anesthesiology 2006; 34: 165-179.
- Scholz A, Mechanisms of (local) anaesthetics on voltage-gated sodium and other ion channels. Br J Anaesth 2002; 89: 52-61
- Stehr S, Ziegeler J, Pexxa A, et al, The effects of lipid infusion on myocardial function and bioenergetics in L-bupivacaine toxicity in the isolated rat heart. Anesth Analg 2007; 104: 186-192.
- Berde C, Toxicity of local anesthetic in infants and children, The Journal of Pediatrics, 1993, 122:14-20.
- Thompson PD et al, Lidocaine pharmacokinetics in advanced heart failure, liver disease and renal failure in humans. Ann Intern Med 1973; 78:499-508.
- Rosenberg PH, Veering BTh, Urmey WF, Maximum recommended dose of local anesthetic: a multifactorial concept. Reg Anesth and Pain Med 2004; 29: 564-575
- Tucker GT, Moore DC, Bridenbaugh PO, et al, Systemic absorption of mepivacaine in commonly use block procedures. Anesth Analg 1972; 37:277-287
- Gitman M, Barrington MJ, Local anesthetic systemic toxicity: a review of recent case reports and registries, Reg Anesth and Pain Med. 2018; 43:124-130.
- Neil JM, Barrington MJ, Fettiplace MR, et al, The third American society of regional anesthesia and pain medicine practice advisory on local anesthetic systemic toxicity, Reg Anesth and Pain Med, 2018; 43: 113-123.
- Barrington MJ, Kluger R, Ultrasound guidance reduces the risk of local anesthetic systemic toxicity following peripheral nerve blockade. Reg Anesth and Pain Med 2013; 38:289-299
- McEvoy MD, Hand WR, Stoll WD, et al, Adherence to guidelines for the management of local anesthetic systemic toxicity is improved by an electronic decision support tool and designated “reader”, Reg Anesth and Pain Med, 2014; 39:299-305
- Fettiplace MR, Weinberg G, The mechanisms underlying lipid resuscitation therapy, Reg Anesth Pain Med 2018; 43: 138-149.