Authors: Rita Agarwal, MD, FAAP, FASA and Julie Good, MD, FAAP: Stanford University School of Medicine - Stanford, CA
18 y.o man with incurable, recurrent metastatic Ewing Sarcoma presents acutely with severe abdominal pain. His abdomen is distended, and a mini laparotomy reveals diffuse intraabdominal metastasis and inoperable multi-location bowel obstruction. At a post-operative care discussion, he and his family express a primary goal of better pain control, and the patient further states he wants to be more alert. The patient is currently on Hydromorphone PCA 500 mCg per hour basal rate, 300 mCg demand dose with 8-minute lockout, Celebrex 200 mg po bid, gabapentin 1200 mg po tid and acetaminophen 650 mg po every 6 hours. The worst pain is in his bilateral lower abdominal and pelvic area which he rates as 8/10. He is DNAR/DNI and is unable to move much due to pain. He can’t sit up in bed, nor can he comfortably lie on his side. His INR is 1.4.
The patient, family and oncologists are requesting a regional technique to help manage his pain.
All of the following interventions should be considered EXCEPT:
Correct!
Wrong!
Question of the Month - October 2022
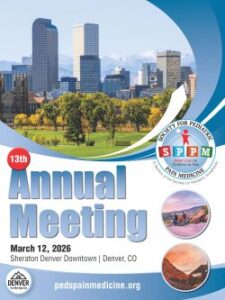 SPPM 13th Annual Meeting
SPPM 13th Annual Meeting