What is Pain?
Pain is an unpleasant sensory and emotional experience typically caused by, or resembling that caused by, actual or potential tissue injury.
- Pain is always a subjective experience that is influenced to varying degrees by biological, psychological, and social factors.
- Experience of pain and the physical sensation of pain are two different phenomena: the experience of pain involves more than just the physical sensation of pain felt by the nerves because of an injury.
- Through their life experiences, individuals learn the concept of pain, its meaning, applications and interpretation.
- A person’s report of an experience as pain should be accepted as such and respected.
- Although pain usually serves a protective role to prevent further damage, it may have adverse effects on function and social and psychological well-being.
- Verbal description is only one of several behaviors to express pain; inability to communicate does not negate the possibility that a human or a non-human animal experiences pain.
This is taken from the International Association for the Study of Pain website: https://www.iasp-pain.org/PublicationsNews/NewsDetail.aspx?ItemNumber=9218
The degree/magnitude of the tissue injury or even absence of any injury, does NOT correlate with the amount of pain and suffering experienced by an individual. The amount of pain and suffering experienced will vary between individuals and over time in any one individual.
What is Acute Pain?
Acute pain usually comes on suddenly and is caused by something specific like an injury, illness like appendicitis, broken bones or surgery. It is usually sharp in quality. It goes away when the underlying cause for the pain gets better. It usually signals that something is wrong and should be protected. Acute pain does not usually last longer than 2-6 weeks.
Common causes of acute pain include:
- Surgery
- Broken bones
- Dental work
- Burns or cuts, bruises
- Infections
Because sudden tissue injury generally causes pro-inflammatory agents to be released, antiinflammatory strategies are often helpful in the treatment of acute pain.
Common ways to treat acute pain include:
- Rest
- Splint/support
- Heat/Ice
- Medications
- Surgery
- Local anesthesia and/or nerve blocks
What is Chronic Pain?
Chronic pain is pain that lasts longer than 3 months and can continue even after the injury or illness that caused it has healed or gone away. Pain signals remain active in the nervous system for weeks, months, or years even if all the tests are normal. Sometimes people suffer chronic pain even when there is no obvious past injury or apparent body damage. This type of pain is no longer protective and does not always mean that there is something wrong.
Chronic pain is usually linked to conditions like
- Headache
- Arthritis
- Cancer
- Nerve pain
- Back pain
- Fibromyalgia pain
People, including children who have chronic pain can have physical and emotional effects that are stressful on the body. Physical effects include tense muscles, limited ability to move around, a lack of energy, and appetite changes. Emotional effects of chronic pain include depression, irritability, anger, anxiety, and fear of re-injury. Such a fear might limit a person’s ability to return to their regular work, school or leisure activities.
Treatment of chronic pain requires a multidisciplinary treatment plan, addressing both the physical and emotional effects. This means your child will be evaluated by many different professionals. Usually your child will be seen by a pain physician, physical therapist, pain psychologist, and sometimes an occupational therapist. Treatment will typically include medications, psychological treatments, pain coping and relaxation strategies, physical and/or occupational therapy as well as other techniques like acupuncture/acupressure, massage, TENS unit etc.
Medications that help the nerve (pain) signals and the nervous system return to normal are more beneficial than medicines that are commonly used for acute pain (opioids).
Can SPPM see/treat my child?
SPPM is not a healthcare facility, therefore it does not offer any direct treatment or clinical care to patients. It is a professional organization made up of healthcare professionals from many different specialities who take care of children’s pain in their own hospitals and clinics.
Can SPPM recommend pain doctors, clinics, or other programs for my child’s pain
SPPM can provide a list of multidisciplinary pediatric pain programs within the United States and internationally, that offer assessment and treatment of pediatric chronic pain conditions. This list is developed and maintained by Tonya Palermo, PhD, based on information provided voluntarily by each of the programs. This list is meant to serve as a resource guide for patients and families in locating a pediatric pain treatment program that may serve their needs based on their location or treatment needs. However, provision of this list should not be viewed as an endorsement of any programs.
How does SPPM advocate for pediatric pain management?
The Society for Pediatric Pain Medicine is a professional organization dedicated to providing better care for children in pain, through clinical care, education, research and advocacy. As a Society, we are committed to learning, discovering, advancing and disseminating information, and education that improves pain management in children. As a professional society, we voice concerns related to children’s pain management, and ensure that policies and regulations around children’s pain issues use the best possible evidence. However, SPPM does NOT provide any direct clinical care or medical advice to patients and families.
We are on a long waiting list to see a pediatric pain specialist/treatment program. Can SPPM help us get an appointment sooner?
SPPM cannot help you change the time of your appointment.. However, you may be able to find another pediatric pain clinic that can see you sooner . Link to multidisciplinary pediatric pain programs
We do not like/agree with the plan of care suggested by my child’s pain provider, can SPPM help with a different plan of care?
SPPM is not a healthcare facility and can not offer any direct treatment or clinical care to patients. SPPM is an organization dedicated to providing better care for children in pain, through clinical care, education, research, and advocacy. Based on the available research we can offer some general guidelines around pediatric pain and its treatment.
Acute pain, such as that related to surgery, is usually treated with medications that commonly include: acetaminophen (Tylenol), ibuprofen (Advil, Motrin), ketorolac, other non-steroidal anti-inflammatory medications, and sometimes opioids (oxycodone, morphine, fentanyl etc.). Local anesthesia and nerve blocks may be used and can be very helpful. The specific type of pain medications or techniques used will depend on the surgery or injury and the resources that hospital or clinic has. It is important to discuss your child’s pain control techniques with your physicians.
Chronic pain is a complex condition resulting from both physical as well as emotional factors. Moreover, it can affect all aspects of a person’s life (physical, social, mental, emotional and even financial). (See Chronic Pain above) Therefore any treatment plan needs to take into account the cause and impact of the pain condition. Treatment may include medication, and/or psychological support and strategies to manage pain, emotions, stress, anxiety, and also ways to help restore your child’s physical abilities and function. Physical and/or occupational therapy is often extremely important in your child’s recovery. We commonly call these as multidisciplinary treatments. The intensity of the treatment program depends on the degree of the disability and dysfunction caused by the pain condition.
What is a multidisciplinary Pain Rehabilitation Program?
The focus of a multidisciplinary pain rehabilitation program often is to help your child regain normal function along with trying to reduce the pain symptoms. Such a program should include considerations of all treatment elements: medications, psychological support and techniques, physical/occupational therapy to address any physical and functional limitations related to pain. There are different types of pain rehabilitation programs, offering outpatient treatments anywhere from a few days a week to daily rehabilitation and sometimes even needing inpatient admission to be most effective.
Why is my child still in pain, when all the tests are “normal”?
“Normal tests” do not mean that your child does not have pain. Most people think of pain as being caused by an injury, illness, or surgery. This is true in acute pain and the pain usually goes away when healing occurs, usually within days to weeks.
Chronic pain is pain that lasts longer than 3 months and may still be present even after the signs of original injury, illness or surgery are long gone. This is because with chronic pain, the nervous system (nerves and the brain) somehow change and continue to send and sense pain signals even after the original problem has healed. There are also some conditions like headaches, migraine, stomachaches etc. where the physical signs of a problem cannot be seen on any tests. The nerves that carry the pain signals from the body to the areas of the brain which sense pain, can continue to send these signals even if there is no injury or damage.
Unfortunately, there are no tests that can simply show us that the nerves are carrying pain signals. Therefore, “normal tests” only means that there is no obvious physical sign that can explain or be fixed to treat the pain your child is experiencing. It means that there are other explanations like the changed nature of the nerves that may need to be addressed to treat your child’s pain.
How do I know my child’s pain treatment is working?
Pain is a complex and personal experience. We have no way to measure pain, so we have to rely on patients’ own report of how much pain they are in. Since there is no objective way to know about patients’ pain and suffering, instead looking at how much the pain is interfering with their ability to function in and enjoy normal life gives the measure of their pain. For children, we look at whether they are able to go to school, do regular activity or chores, get regular exercise, and spend time with friends and family. When those goals are not being met, we try to understand what the obstacles are and work with the patients and their families to try to overcome them. Practically, often patients need to return to some degree of normal function before their pain improves or resolves. Limiting activities or waiting to resume them until their pain goes away, generally only prolongs and worsens pain and suffering.
Are there other types of treatments besides medications? How would they help my child’s pain? Why does my child have to see a psychologist, when they have a physical condition causing their pain?
Medications are only one way of helping with pain. It is well known that the same pain condition can be experienced differently by different individuals. This is because pain is a complex condition, affected by both the body and the mind. While pain usually starts with unpleasant sensation because of a physical trauma/injury or inflammation at body sites, these sensations can feel much worse if there is an expectation of suffering.
Sometimes previous experience, horror stories from well-meaning friends and relatives can increase this expectation and increase anxiety. There are many things that influence how a child experiences the pain, like the mental framework of the child – worries, sadness, anxiety, depression, child’s personality, previous bad experience(personal or of someone they know) – and even some of other stressors from school or family can worsen their experience of pain. These things can create a mismatch between the degree of pain which is related to the physical injury or damage and what is actually being experienced by the patient. Thus, a psychologist can teach the child and the family techniques to understand and recognize the effects of all these factors on the child’s pain and can teach techniques and effective ways to calm the mind, decrease anxiety, worry, stress etc. and thus decrease the influence from these factors on your child’s pain. These are important ways to decrease the experience of pain. Psychologists, holistic care practitioners, integrative care specialists etc. are experts who can either teach or offer children different techniques, like cognitive behavioral therapy, breathing techniques for pain relief, calming/relaxing the mind and therefore help decrease the pain experience and/or help the child return to a more functional life. This allows the child to have a better quality of life and not have their, and your life be totally consumed by the painful condition.
Why does my child have to see a physical therapist/occupational therapist when this makes their pain worse?
Pain limits the ability of a child to do normal activities, play or be active. Sometimes the child or a parent may limit themselves because of the worry of making the pain worse due to activity and stop all activity until the pain gets better. Although this may be a helpful and protective thing in case of acute injury/pain, for chronic pain, it sends the wrong signals to the brain and usually makes things worse. Limiting the activity, can cause the muscles to tighten, loose their function and strength, this can make the pain worse and hence causing a vicious cycle of pain and disability. A physical or occupational therapist can teach your child how to safely and slowly restart activity, what types of activities are safe and helpful, how to gradually increase the activity, build strength and return to normal function. They may give your child a home exercise program in addition to some sessions in their office. It is important to follow through both of those.
Moreover, doing physical activity, especially guided by a PT/OT, helps the body produce its internal pain fighting chemicals (endorphins) and feel good hormones (dopamine), which also help decrease your child’s pain.
Will my child get addicted to pain medications?
It’s important to know that addiction is very rare for children who take medications to relieve their pain especially supervised by their doctor.
There are some medications that can cause the body to become used to them when used for long periods of time, like the opioids (morphine, oxycodone etc.) or benzodiazepines (diazepam, lorazepam etc.) class of medications, if used long term. These medications are usually used for treatment of acute pain and are usually safe when used appropriately, supervised by your child’s doctor.
Your child’s healthcare team should work with you and watch your child’s pain medication and doses carefully to be sure the medicine is safe and right for him/her. Be sure to let your doctor, nurse or pharmacist know if you have any questions or concerns.
Can we use alternative medicine treatments while my child is being treated for pain?
Usually. A lot of alternative medicine treatments have limited or sometimes conflicting evidence to support their use in pain management. There is excellent evidence for use of a number of “non-medical” therapies for a variety of acute and chronic pain problems.
Therefore, they have become regarded as mainstream pain management therapies by most healthcare professionals. These include therapies like –
- Cognitive and behavioral therapies (CBT), Biofeedback, Relaxation and other biobehavioral therapies
- Transcutaneous electrical nerve stimulation (TENS)
- Acupuncture
- Massage
Yoga also has many studies showing its benefit for back and other musculoskeletal pain conditions. While chiropractic care has a number of studies showing efficacy for low back pain, it should be considered carefully for other conditions. Herbal remedies and dietary supplements should be treated as medications as they often have active ingredients with distinct pharmacologic effects.
Talk to your physician about the use of alternative medicine treatments and any possibility of harmful interactions between their medical treatments and use of ant alternative therapies including any herbal remedy or dietary supplement you might consider.
How do we know which alternative treatment to use?
Although most alternative medical treatments are low risk (with the possible exception of some herbal remedies), It is important to discuss with your child’s pain doctor, if you are considering or using any alternative therapies.
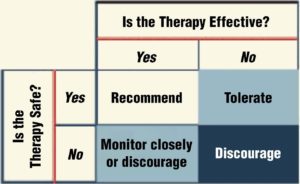
No therapy will help all patients who use it. If it is helpful and not causing harm, it is probably reasonable to continue.
Here is a guide you or your doctor may follow when thinking about using alternative treatments:
Many alternative therapies are not covered by insurance, however, so there will likely be a financial burden and you may need to check with your insurance company first. There may also be an added time burden from the alternative treatment visits and if they take away from the use of more proven therapies such as cognitive and behavioral therapy or physical therapy and exercise, that is a potential problem.
How do I store my child’s medications?
All medicines should be stored safely away from children. Controlled substances, such as oxycodone or valium should be kept in a secure location at all times. A locked box or cabinet is best, but if that is not possible then make sure the medications are hidden and out of reach. Toddlers are curious and may think medicine is candy and will put it in their mouths. Teenagers (or their friends, neighbors, or relatives) may be curious as well and should be protected from the temptation to experiment.
What do I do with/How should I dispose of the leftover medications?
All leftover medications should be properly disposed using FDA guidance.
disposal-unused-medicines-what-you-should-know
The FDA recommends returning unused medications as soon as possible. There are 2 ways to find the nearest location that will take back medications. The nearest locations can be found at this FDA site, which includes a link to the DEA Diversion Prevention Site and a link to Google Maps with nearby locations marked https://www.fda.gov/drugs/disposal-unused-medicines-what-you-should-know/drug-disposal-drug-take-back-locations
If there are no places nearby to easily and safely return drugs, the FDA has a Safe Flush List of medications that can be flushed down the toilet.
Since many people do not like to flush medications into the water supply, other options are to mix the medication in kitty litter, used coffee grounds, washing powder or something else that cannot be ingested, sealing it in a plastic bag and throwing it in the trash. Some clinics and Doctors may give you a kit to safely dispose of leftover medications. If so, carefully follow the directions on the kit to safely inactivate and dispose of the medication.
Pharmacies are not allowed, by law, to re-prescribe used or returned medications. They cannot offer a refund on unused medications.
It is illegal to save prescription medications for use at a time other than the episode for which they were prescribed. Use at any other time by any person, even the person that they were originally prescribed for, is considered diversion by the federal Drug Enforcement Agency.
I have another question.
Didn’t find an answer to your question? Contact us.
