ASA Presentations
Combined Spinal Caudal Anesthesia in Infants: Case Report and Literature Review
By Johanna M. Lee, MD; Chang Amber Liu, MD, MSc
Department of Anesthesia, Critical Care and Pain Medicine
Massachusetts General Hospital, Harvard Medical School
Boston, Massachusetts
INTRODUCTION
Spinal anesthesia has been shown to be safe and effective in infants, and has been gaining popularity as an alternative to general anesthesia for infants undergoing urologic and abdominal surgeries.1-3 Continuous regional anesthesia via caudal catheters has also been shown to be safe and effective in infants.4-7 Regional anesthesia in infants has several benefits, including the avoidance of intubation and associated possible respiratory complications, ability to avoid opioids and decrease early postoperative apneic events, and improved hemodynamic stability.8,9 These benefits are of particular consideration in high-risk patients, notably ex-premature infants with cardiac, pulmonary, or neurologic comorbidities.1-3
Spinal anesthesia has been shown to improve OR and PACU efficiency compared with general anesthesia, using a standardized protocol for infants undergoing inguinal herniorrhaphy at Massachusetts General Hospital for Children.1,10 Spinal anesthesia is also associated with a decrease in postoperative rFLACC scores and acetaminophen consumption.11 While there have been concerns that spinal anesthesia in infants can be technically challenging, spinal anesthesia has been shown to be feasible and have a high success rate (greater than 90%).1,3,12
While spinal anesthesia has many benefits over general anesthesia for certain types of surgeries, it is limited by its short duration of approximately 60-90 minutes in infants.1,13 The addition of adjuncts like epinephrine and clonidine can extend the duration of block up to 120 minutes,10,12,13 but still would not be sufficient for longer procedures. Data from studies of spinal anesthesia in infants have shown that approximately 1% of patients needed conversion to general anesthesia because of insufficient duration of spinal anesthesia.1,3
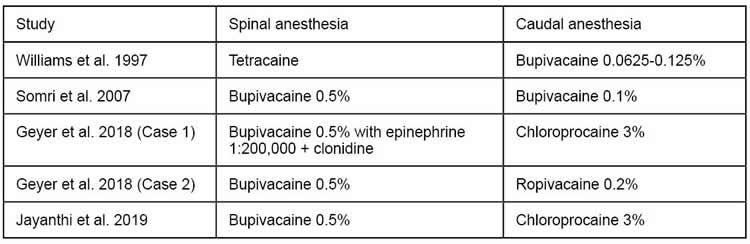
Over the years, there have been a number of reports of combined spinal and caudal/epidural anesthesia in infants undergoing prolonged surgical procedures, with a proportion requiring supplemental sedative intravenous medications (Table 1).14-17 While older studies tended to use bupivacaine infusions, more recent studies have incorporated the use of chloroprocaine infusions, which have a better safety profile due to its short plasma half-life (Table 2).4 The rate of complications and rate of conversion to general anesthesia are very low.
CASE REPORT
We present the use of awake combined spinal caudal (CSC) anesthesia in a full-term 9-week old with a history of congenital hydroureteronephrosis, who was scheduled for a cystoscopy and possible stent placement versus ureteral reimplantation. She weighed 6.15 kg, had no allergies, and was otherwise healthy. Given parental concerns with the patient’s prior post-intubation complications, we opted to avoid airway instrumentation, and given the uncertainty of procedural duration, proceeded with spinal anesthesia followed by placement of a caudal catheter, based on our previously published spinal anesthesia protocol10 and the protocol for caudal anesthesia outlined by Geyer et al.16
Briefly, topical local anesthetic was applied to the lumbar spine in the pre-operative area. In the operating room, the patient was seated with the help of an assistant, and after sterile preparation, the intrathecal space was accessed using a 22G Quincke spinal needle. On return of CSF, 1 mg/kg bupivacaine 0.5% and 1 mcg/kg of clonidine were administered. An IV was placed in the lower extremity, and then placed in right lateral decubitus position for epidural catheter placement. The caudal space was accessed using a 20G needle, and a caudal catheter was advanced into the epidural space and through this needle. After a negative test dose, the catheter was secured with a drop of Dermabond at the entry site, Tegaderm, then tape. The patient was repositioned supine for the operation and was given Sweet-Ease for comfort throughout the case. The patient did not require any additional IV sedatives.
At approximately 75 minutes, we noticed increased fussiness, and the caudal catheter was incrementally bolused over 5 minutes with 1 ml/kg chloroprocaine 2% with good effect. We subsequently started a chloroprocaine 2% infusion at 1 ml/kg/hr. The procedure lasted approximately 3 hours, and the patient did not require supplemental IV sedation. She underwent an uneventful recovery in the post-anesthesia care unit (PACU), and the caudal catheter was used for postoperative analgesia with a continuous ropivacaine infusion with good effect. The caudal catheter was removed on post-operative day 2 without complications.
DISCUSSION
Spinal and caudal anesthesia, as well as combined spinal caudal anesthesia, have been shown to be safe and effective in infants undergoing urologic and major abdominal surgeries. While early studies focused on high-risk patients, this technique can be used effectively in otherwise healthy ASA I or II infants. Combined spinal caudal anesthesia, particularly when incorporated into a standardized program in collaboration with the surgical team, can be a viable alternative to general anesthesia for prolonged infraumbilical procedures, can provide effective postoperative analgesia, and has the potential to improve OR efficiency. The addition of postoperative analgesia via a caudal catheter can be particularly beneficial for high-risk patients, as this can reduce the need for supplemental opioids during their recovery period and hospitalization. While a review of the literature shows that a large proportion received supplemental sedation with midazolam or dexmedetomidine (or, uncommonly, propofol), there may be substantial variation depending on the institution and the age of the patients. We submit that for younger infants who are less than 6 months of age, the use of Sweet-Ease may allow them to tolerate surgery under spinal/caudal anesthesia without additional IV sedation.
Table 1. Summary of Studies of Combined Spinal and Caudal/Epidural Anesthesia in Infants.
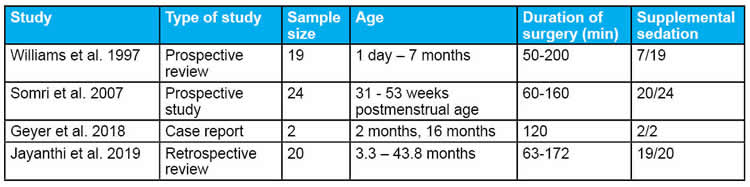
Table 2. Summary of Local Anesthetic Choice for Combined Spinal-Caudal Anesthesia.
REFERENCES
- Williams RK, Adams DC, Aladjem EV, et al. The safety and efficacy of spinal anesthesia for surgery in infants: The Vermont Infant Spinal Registry. Anesthesia and Analgesia 2006;102:67-71.
- Jones LJ, Craven PD, Lakkundi A, et al. Regional (spinal, epidural, caudal) versus general anaesthesia in preterm infants undergoing inguinal herniorrhaphy in early infancy. Cochrane Database of Syst Rev 2015;6:CD003669.
- Kachko L, Simhi E, Tzeitlin E, et al. Spinal anesthesia in neonates and infants – a single-center experience of 505 cases. Pediatric Anesthesia 2007;17:647-53.
- Henderson K, Sethna NF, Berde CB. Continuous caudal anesthesia for inguinal hernia repair in former preterm infants. J Clin Anesth 1993;5:129-133.
- Tobias JD, Lowe S, O’Dell N, et al. Continuous regional anaesthesia in infants. Can J Anaesth 1993;40(11):1065-8.
- Calder A, Bell GT, Anderson M, et al. Pharmacokinetic profiles of epidural bupivacaine and ropivacaine following single-shot and continuous epidural use in young infants. Paediatr Anaesth 2012;22(5):430-7.
- Mueller CM, Sinclair TJ, Stevens M, et al. Regional block via continuous caudal infusion as sole anesthetic for inguinal hernia repair in conscious neonates. Pediatr Surg Int 2017;33(3):341-345.
- Davidson AJ, Morton NS, Arnup SJ, et al. Apnea after awake regional and general anesthesia in infants. Anesthesiology 2015;123(1):38-54.
- McCann ME, Withington DE, Arnup SJ et al. Differences in blood pressure in infants after general anesthesia compared to awake regional anesthesia (GAS study – a prospective randomized trial). Anesthesia and Analgesia 2017;125(3):837-45.
- Liu CA, Davis N, Kelleher CM. Application of an infant spinal anesthesia protocol in infants presenting for inguinal herniorrhaphy improves operating room and postoperative recovery unit utilization. Pediatric Anesthesia 2019;29(8):881-882.
- Chen FK, Li LT, Kelleher CM, Liu CA. Infant spinal anesthesia reduces postoperative pain scores and pain medication consumption in infants undergoing inguinal herniorrhaphy. Journal of Pediatric Surgery 2020;S0022-3468(20)30589-3.
- Whitaker EE, Wiemann BZ, DaJusta DG, et al. Spinal anesthesia for pediatric urological surgery: Reducing the theoretic neurotoxic effects of general anesthesia. Journal of Pediatric Urology 2017;13:396-400.
- Trifa M, Tumin D, Whitaker EE, Bhalla T, Jayanthi VR, Tobias JD. Spinal anesthesia for surgery longer than 60 min in infants: experience from the first 2 years of a spinal anesthesia program. Journal of Anesthesia 2018;32:637-40.
- Williams RK, McBride WJ, Abajian JC. Combined spinal and epidural anaesthesia for major abdominal surgery in infants. Can J Anaesth 1997;44(5):511-514.
- Somri M, Tome R, Yanovski B, et al. Combined spinal-epidural anesthesia in major abdominal surgery in high-risk neonates and infants. Pediatric Anesthesia 2007;17:1059-65.
- Geyer ED, Martin DP, Bhalla T, et al. Combined spinal and caudal epidural anesthesia for prolonged surgical procedures in pediatric-aged patients: A report of two cases. J Med Cases 2018;9(2):64-67.
- Jayanthi VR, Spisak K, Smith AE, et al. Combined spinal/caudal catheter anesthesia: Extending the boundaries of regional anesthesia for complex pediatric urological surgery. Journal of Pediatric Urology 2019;15(5):442-447.




