ASA Presentations
Retrospective Evaluation of Opioid-Sparing Multimodal Analgesia Regimen for Postoperative Pain Control during Tonsillectomy with and without Adenoidectomy
By Andrew G. Rudikoff, MD1; Robert L. Rettig, MD2; David D. Tieu, MD3; Carolyn V. Nguyen, MD3; Franklin M. Banzali, MD1; Marlene M. Nashed, Pharm.D4; Janet Mora-Marquez5; Qiaoling Chen, MS5; Antonio Hernandez Conte, MD, MBA, FASA1
1Department of Anesthesiology, 2Department of Surgery, 3Department of Head & Neck Surgery, 4Department of Pharmacy, Kaiser Permanente Los Angeles Medical Center, Los Angeles, California, 5Department of Research & Evaluation, Kaiser Permanente Southern California, Pasadena, California
INTRODUCTION
Tonsillectomy with and without adenoidectomy is one of the most common pediatric surgeries performed in the United States; recent incidence is 289,000 per year.1 Adenotonsillar hypertrophy causing obstructive sleep apnea (OSA) is the most common indication for this operation; an additional indication includes chronic tonsillitis. Pain control is critical after these surgeries, and patients with OSA are exquisitely sensitive to opioids, the most commonly used medication for acute postsurgical pain. Thus, patients undergoing tonsillectomy and adenoidectomy (T&A) are at increased risk of postoperative respiratory complications, along with opioid related side-effects including nausea, vomiting, constipation, pruritis, and even death.2
Since 2016, our integrated health care system has implemented a comprehensive multimodal analgesic regimen for our pediatric patients undergoing tonsillectomy with and without adenoidectomy as part of an opioid sparing initiative in our health system.
The opioid-sparing regimen consists of perioperative acetaminophen and dexmedetomidine, and postoperative standing doses of acetaminophen and ibuprofen. Our retrospective study sought to compare the multimodal analgesic regimen (MMAR) initiated in 2016 with a matched population prior to 2016 who did not receive the MMAR.
We hypothesized that a formal MMAR for perioperative pain control among patients undergoing tonsillectomy with and without adenoidectomy would lead to decreased post-anesthesia care unit (PACU) opioid use, decreased PACU and postoperative pain scores, decreased PACU length-of-stay (LOS), reduced utilization of opioids at home, and decreased readmissions to the emergency room for pain.
METHODS
This study utilized a retrospective review of existing patient electronic medical record database from January 1, 2013 to December 31, 2018. International Classification of Diseases-9 (ICD) and ICD-10 codes were utilized to identify patients who underwent tonsillectomy with and without adenoidectomy. Patients undergoing tonsillectomy (with and without adenoidectomy) who received an opioid-sparing analgesic regimen were compared to matched controls having received traditional unrestricted opioid-based analgesic regimen. The control and study subjects were divided into two additional sub-cohort groups based on age: 1) 0-7 years of age and 2) 8-13 years of age.
The primary outcome measure was administration of rescue opioids in the PACU. Secondary outcome measures included recovery room time length-of-stay (minutes), hospital LOS (hours), postoperative prescription (yes/no) and dispensation (yes/no) of opioids at home, and readmissions to the emergency room for pain or hemorrhage (yes/no).
RESULTS
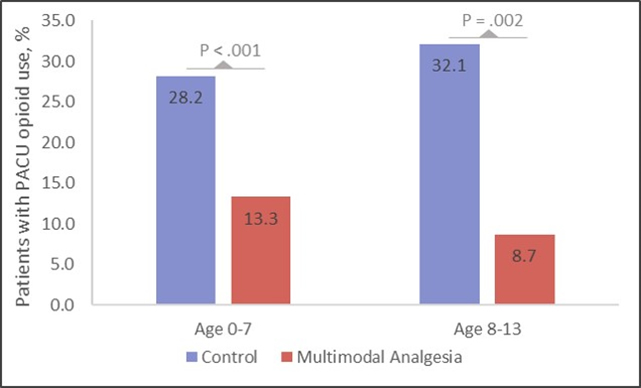
Figure 1 is a stacked bar plot that graphically highlights opioid consumption expressed as percent administered to the control and MMAR groups.
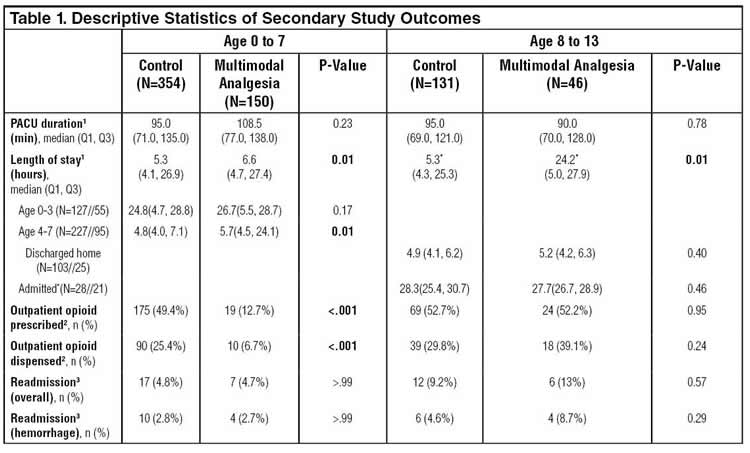
Table 1 summarizes PACU duration, hospital LOS, outpatient opioids prescribed and dispensed, and readmission rates.
DISCUSSION
By using perioperative acetaminophen, dexmedetomidine, and lowered fentanyl dosing, coupled with home utilization of ibuprofen and acetaminophen, we have demonstrated both opioid reduction in the perioperative period and reduced opioid prescriptions and dispensations when the patient transitioned home. There was no difference in PACU length-of-stay between both groups for patients who were discharged the same day or admitted to the hospital. The age 4-7 and age 8-13 cohort of patients who did leave the same day did not have delayed discharge, indicating that the potentially sedative effects of dexmedetomidine in the PACU did not delay discharge.
In the 0 – 7 age MMAR group, there was reduced opioid prescription utilization when the patient was discharged home, likely due to the standing doses of acetaminophen and ibuprofen. Combining these two medications yields synergistic action to provide effective analgesia for many patients undergoing tonsillectomy with and without adenoidectomy. Fewer surgeons prescribed opioids to their MMAR patients, and fewer parents went to our institution’s pharmacy to retrieve them. This reduction was a concerted effort by our institution to reduce home administration opioids in this patient population. However, in the 8-13 group, there was no difference in the amount of opioids prescribed and dispensed between both groups. We cannot account for this phenomenon. It may be that patients aged 8-13 experience a higher degree of discomfort due to the surgery itself, or it may possibly be due to bias from parents who are more willing to administer opioids to older children than younger children. Complication rates were similar in both groups, and both groups had similar readmissions for pain and for hemorrhage.
ACKNOWLDGEMENTS
None
FUNDING
This study was supported by a grant from Kaiser Permanente #RRC-20181102.
CONFLICT OF INTEREST
The authors report no conflicts of interest.
AUTHOR CONTRIBUTION
AGR, RLR, DDT, CVN, FMB, AHC conducted background research, conducted the study, interpreted the results and co-wrote/edited the manuscript. JMM, MMN and QC conducted the statistical analysis, interpreted the results and co-wrote/edited the manuscript.
ORCID
Antonio Hernandez Conte: https://orcid.org/0000-0002-9335-462X
REFERENCES
- Hall MJ, Schwartzman A, Zhang J, Liu X. Ambulatory surgery data from hospitals and ambulatory surgery centers: United States, 2010. National Health Statistics Reports. 2017(102):1-15.
- Coté CJ, Posner KL, Domino KB. Death or neurologic injury after tonsillectomy in children with a focus on obstructive sleep apnea: Houston, we have a problem! Anesthesia & Analgesia. 2014;118




