Update in Pediatric Regional Anesthesia
New Peripheral Nerve Blocks: Are They Worth the Hype?
By Adrian Bosenberg, MBChB, FFA (SA); Erica Holland, MD
Department of Anesthesiology and Pain Medicine
Seattle Children’s Hospital
University of Washington
Seattle, Washington
The advent of portable ultrasound technology has revolutionized our ability to place peripheral nerve blocks within tissue planes. Ultrasound guidance has facilitated the introduction of new innovative approaches to deeper nerves not previously attempted using landmark based techniques. The majority of these blocks involve the branches of the spinal nerves.
A unique feature of truncal nerve blocks is that the nerve per se does not need to be visualized to achieve success. Local anesthetic injected into the correct tissue plane will spread to reach the nerve. The path taken by the nerve and its branches, together with the location of local anesthetic placement, determines the distribution of the block and possibly its duration.
Important considerations when performing these blocks include understanding the path of the nerve(s) and its anatomical relationships along that path, as well as the extent of the sensory, motor, and autonomic distribution of the nerve. The thoracolumbar fascia plays an important role in defining the local anesthetic spread. Spinal nerves, in general, divide into dorsal and ventral primary rami. The dorsal ramus passes through the erector spinae muscle and branches into medial and lateral posterior cutaneous branches. The ventral rami in the thorax pass deep to the intercostal muscles to branch into lateral and anterior cutaneous branches in the chest wall. In the abdominal wall they pass between the internal oblique and transversus abdominis muscles. The rami communicantes branch off the ventral rami anteriorly to join the sympathetic chain.
A variety of approaches have been described for the quadratus lumborum (QL) block, and the erector spinae block (ESP). Both are essentially a more proximal approach to the spinal or intercostal nerve than the transversus abdominis plane (TAP) block. Irrespective of the volume used, spread of local anesthetic is limited and unreliable after a conventional mid-axillary TAP block.
The erector spinae block (ESB) is perhaps the most exciting of the tissue plane blocks described recently. The muscles of the back, i.e. the trapezius, rhomboids (above the level of T7) and the erector spinae form tissue planes that can be visualized with ultrasound and utilized for block placement. ESB is easy to perform and not very time consuming. Local anesthetic placed deep to the erector spinae muscle, adjacent to the transverse process of specific vertebra spreads over more dermatomes than a paravertebral block. Local anesthetic also spreads anteriorly into the paravertebral space where it has the possibility to block the sympathetic chain to provide visceral analgesia, and laterally to block the intercostal nerves. Local anesthetic placed in the ESP between the transverse processes does not seem to affect the spread of local anesthetic. Bilateral ESB behaves like an epidural, and, initial reports suggest that the duration of the ESB is longer than a paravertebral block. The duration of the block can be extended by catheter placement using either continuous infusions or intermittent bolus injections as needed.
The ideal dose for most of the fascial plane blocks in children has yet to be determined. Based on a series of unilateral ESP blocks in infants for gastrostomy placement, at least 5 dermatomes were blocked using 0.5ml/kg of bupivacaine (i.e. 0.1ml/kg/dermatome). In a neonatal cadaver study using 0.1ml/kg dye spread over at least 3 spinal nerves (dermatomes) was noted.
The QL spread differs depending on the approach used. With the lateral approach the local anesthetic agent is placed lateral to the QL and posterior to the thoracolumbar fascia; while with the anterior approach the local anesthetic is placed in the plane between the QL and psoas major muscle with spread into the paravertebral space; and the posterior approach places the local anesthetic posterior to the QL and anterior to the latissimus dorsi. The intramuscular approach places the local anesthetic within the QL muscle and blocks the nerve as it traverses the muscle. Each of these approaches have subtle differences in block distribution.
Are there advantages to the different approaches? Based on studies in adults, and limited series in children, it seems that the closer the local anesthetic is placed to the origin of the nerve (i.e. in the paravertebral space) the spread is wider and covers more dermatomes. The duration also seems to be longer because the paravertebral space may act as a depot. A direct comparison between an ESP (at L1) and QL block (QL4-intramuscular approach) for lower abdominal surgery there was no difference in analgesia. This is not surprising since the same nerve is blocked albeit at different sites. Advantages over an epidural block include the ability to achieve unilateral blocks, to use when epidurals are contraindicated, reduce the potential for urinary retention and patients could be discharged earlier with continuous peripheral nerve catheters in situ.
Serratus anterior nerve block (SAB) is another fascial block that is also gaining popularity in recent years. The serratus anterior muscle originates on the 1st to 8th ribs and inserts along the medial border of the scapula. At the level of the 5th rib the teres major, latissimus dorsi, and serratus muscles can be seen on ultrasound. This block induces analgesia in the anterolateral and posterior chest wall by targeting the lateral cutaneous nerves that lie in the interfascial plane between the serratus anterior and latissimus dorsi muscles. A block may also be successful when placed anterior to the serratus anterior muscle. With the needle entry in the mid-axilla, the tissue plane can be easily identified using ultrasound guidance. The SAB has been used for thoracotomy, sternotomy and other chest wall procedures (breast surgery). A SAB is equally efficacious to an intercostal nerve block for post-thoracotomy pain but is longer lasting (and both do not cover visceral pain).
To make valid comparisons and to avoid confusion, the nomenclature for the different approaches to a particular nerve block need to be standardized. Each block has value, but the safety of each approach has yet to established. Block choice is determined by the surgical site but should also balance the risk and benefits associated with the block. To date the published numbers are small. One pneumothorax has been described in an adult, none in infants and children, after an ESP block. Two children with a coagulopathy have developed a hematoma after a QL block.
In conclusion, ultrasound guided fascial plane blocks represent a rapidly expanding new era in regional anesthesia. Individual nerves do not need to be identified. Instead, ultrasound is employed to identify a target muscular plane into which local anesthetic is injected in such a way that it spreads along the desired fascial plane to anesthetize traversing nerves. Most are straightforward, easy to learn, and quick to perform. Their introduction into clinical practice for both acute and chronic pain has come with a lot of hype as illustrated by the multitude of case reports or small case series that have been published over the past few years. Further investigation is still needed in all age groups to establish the preferred approach, the appropriate age-related dose for each block, and to establish their role in clinical practice and multimodal analgesia.
REFERENCES
- Tsui BCH, Fonseca A, Munshey F, McFadyen G, Caruso TJ. The erector spinae plane (ESP) block: A pooled review of 242 cases. J Clin Anesth 2019: 53:29-34.
- Holland E, Bosenberg A. Early Experience with Erector Spinae Plane Blocks in Children Pediatr Anesth 2020;30(2):96-107.
- Govender S, Mohr D, Van Schoor AN, Bosenberg A.The extent of cranio-caudal spread within the erector spinae fascial plane space using computed tomography scanning in a neonatal cadaver. Paediatr Anaesth. 2020 Apr 8. Online ahead of print.
- Govender S, Mohr D, Bosenberg A, Neels Van Schoor A. The anatomical features of an ultrasound-guided Erector Spinae Fascial Plane block in a cadaveric neonatal sample. Paediatr Anaesth. 2020 Sep 2. Online ahead of print.
- Govender S, Mohr D, Bosenberg A, Van Schoor AN A cadaveric study of the erector spinae plane block in a neonatal sample. Reg Anesth Pain Med. 2020; 45(5):386-388.
- Sato M, Hara M, Uchida O. An antero-lateral approach to ultrasound-guided lumbar plexus block in supine position combined with quadratus lumborum block using single-needle insertion for pediatric hip surgery. Paediatr Anaesth. 2017;27(10):1064-1065.
- Ueshima H, Otake H, Lin JA. Ultrasound-Guided Quadratus Lumborum Block: An Updated Review of Anatomy and Techniques. Biomed Res Int. 2017; 2017:275-287.
- Abdallah FW, Chan VW, Brull R. Transversus abdominis plane block: a systematic review. Reg Anesth Pain Med. 2012; 37(2):193-209.
- Hernandez MA, Palazzi L, Lapalma J, Forero M, Chin KJ. Erector Spinae Plane Block for Surgery of the Posterior Thoracic Wall in a Pediatric Patient. Reg Anesth Pain Med. 2018;43(2):217-219.
- Hernandez MA, Vecchione T, Boretsky K. Dermatomal spread following posterior transversus abdominis plane block in pediatric patients: our initial experience. Paediatr Anaesth. 2017;27(3):300-304.
- Dam M, Moriggl B, Hansen CK, Hoermann R, Bendtsen TF, Børglum J. The Pathway of Injectate Spread With the Transmuscular Quadratus Lumborum Block: A Cadaver Study. Anesth Analg. 2017;125(1):303-312.
- Visoiu M, Yakovleva N. Continuous postoperative analgesia via quadratus lumborum block - an alternative to transversus abdominis plane block. Paediatr Anaesth. 2013;23(10):959-61
- Ueshima H, Hiroshi O. Spread of local anesthetic solution in the erector spinae plane block. J Clin Anesth. 2017; 16:45:23.
- De la Cuadra-Fontaine JC, Concha M, Vuletin F, Arancibia H. Continuous Erector Spinae Plane block for thoracic surgery in a pediatric patient. Paediatr Anaesth. 2018;28(1):74-75.
- Ueshima H, Otake H. Clinical experiences of erector spinae plane block for children. J Clin Anesth. 2018; 44:41.
- Karuppiah N, Pehora C, Haller C, Taylor K Surgical Closure of Atrial Septal Defects in Young Children-A Review of Anesthesia Care in Sternotomy and Thoracotomy Approaches. J Cardiothorac Vasc Anesth. 2020 Jul 9: S1053-0770(20)30653-4. Online ahead of print.
- Macaire P, Ho N, Nguyen V, Phan Van H, Dinh Nguyen Thien K, Bringuier S, Capdevila X.Bilateral ultrasound-guided thoracic erector spinae plane blocks using a programmed intermittent bolus improve opioid-sparing postoperative analgesia in pediatric patients after open cardiac surgery: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med. 2020;45(10):805-812
- Kaushal B, Chauhan S, Magoon R, Krishna NS, Saini K, Bhoi D, Bisoi AK.Efficacy of Bilateral Erector Spinae Plane Block in Management of Acute Postoperative Surgical Pain After Pediatric Cardiac Surgeries Through a Midline Sternotomy. J Cardiothorac Vasc Anesth. 2020;34(4):981-986
- Aksu C, Şen MC, Akay MA, Baydemir C, Gürkan Y.Erector Spinae Plane Block vs Quadratus Lumborum Block for pediatric lower abdominal surgery: A double blinded, prospective, and randomized trial. J Clin Anesth. 2019; 57:24-28.
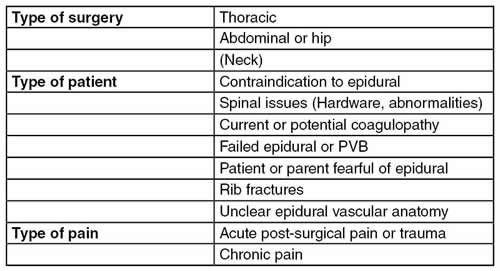
Table 1: Characteristics of fascial plane blocks compared with neuraxial blocks
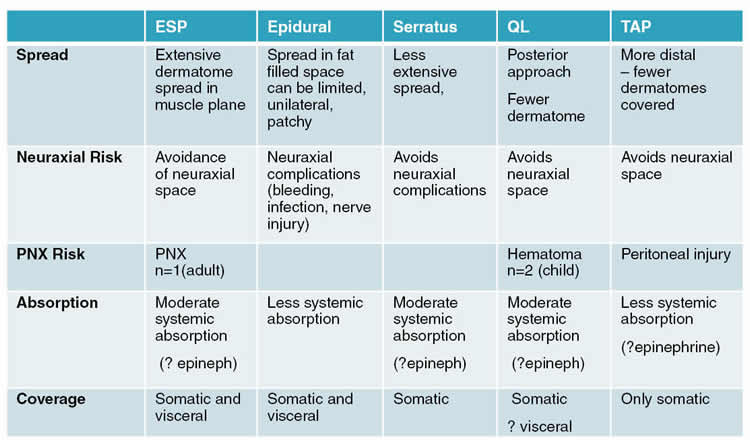
Table 2: Some indications for fascial plane blocks